Heart
Lab Summary
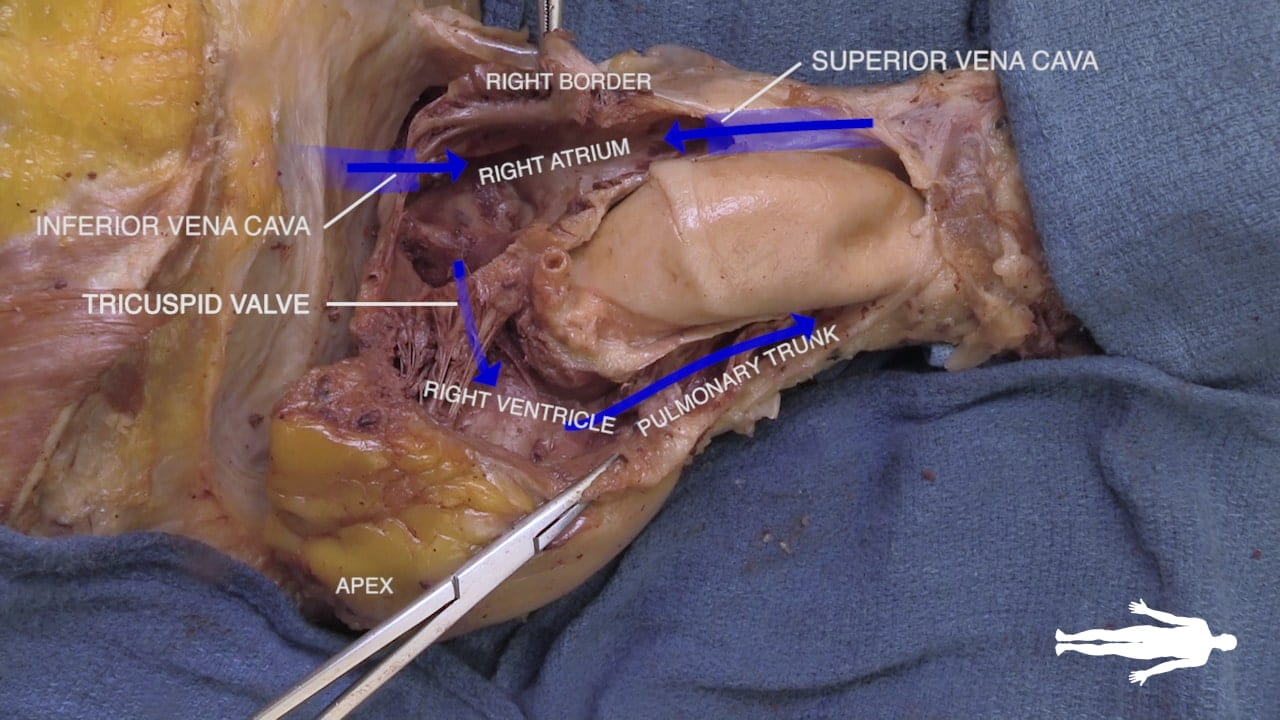
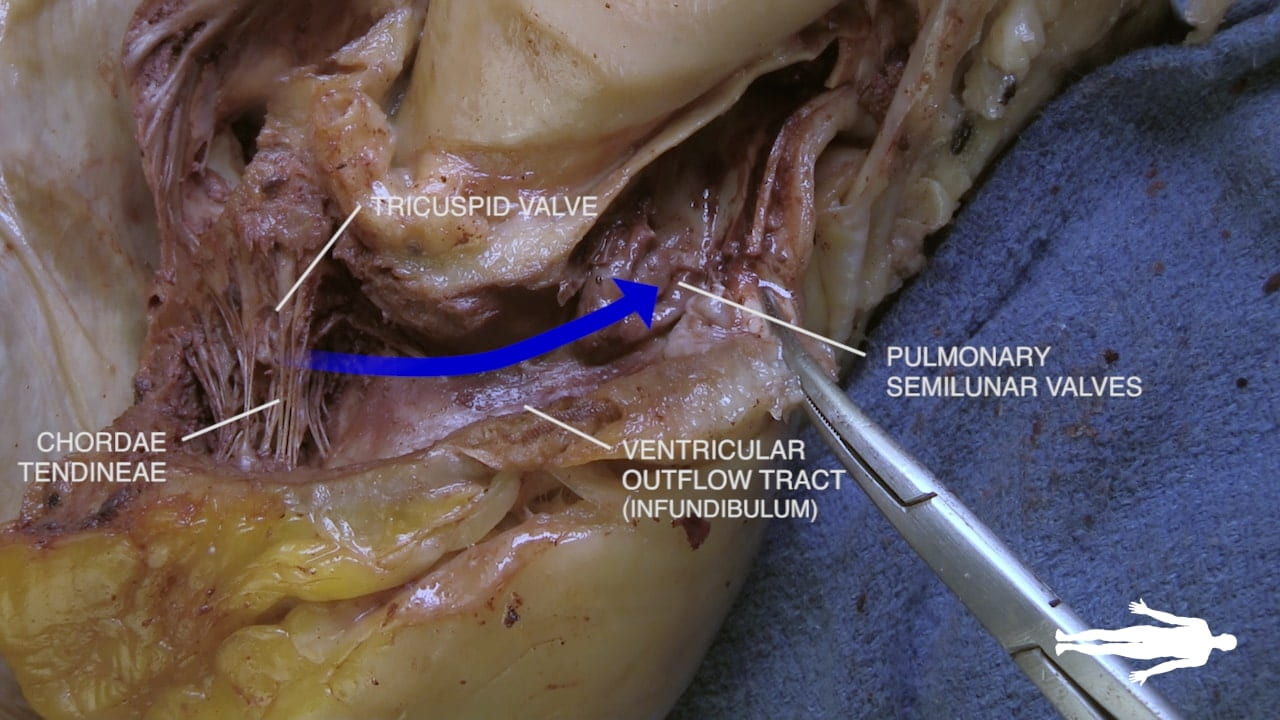
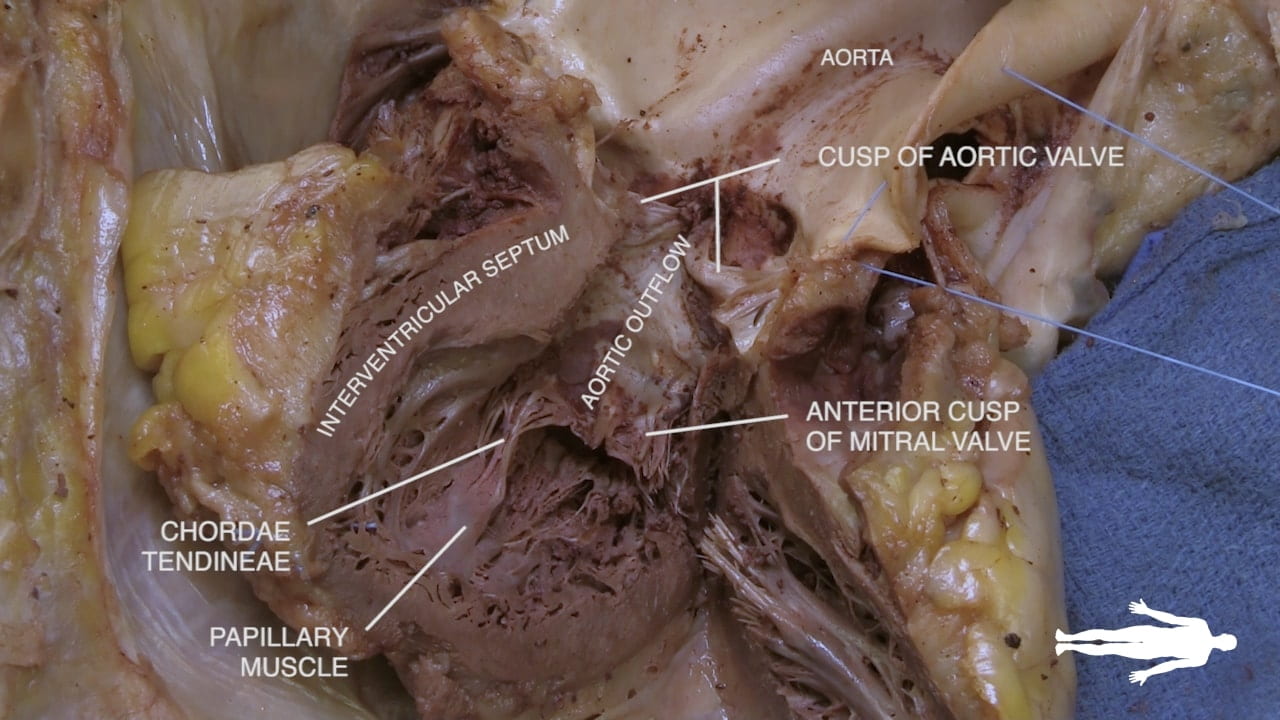
This lab explores the relationships of the heart to surrounding structure and their clinical importance. Cardiac surfaces, the interior structure of the heart and coronary circulation is taught. The interior of the heart is taught through in situ and isolated dissections.
Lab Objectives
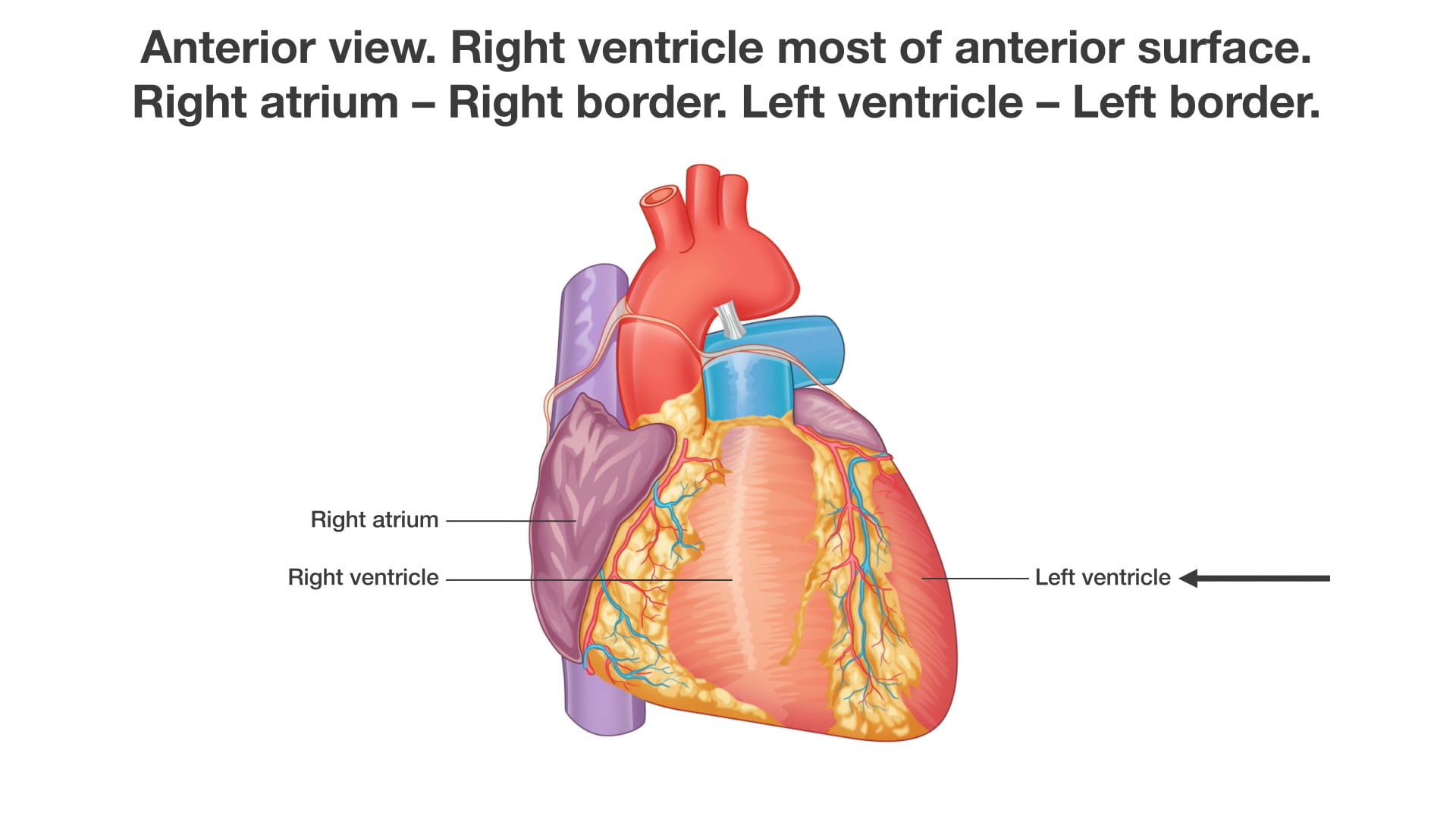
- Describe the chambers of the heart that contribute to the cardiac surfaces and borders.
- Describe the pericardium.
- Explain the significance of the transverse pericardial sinus.
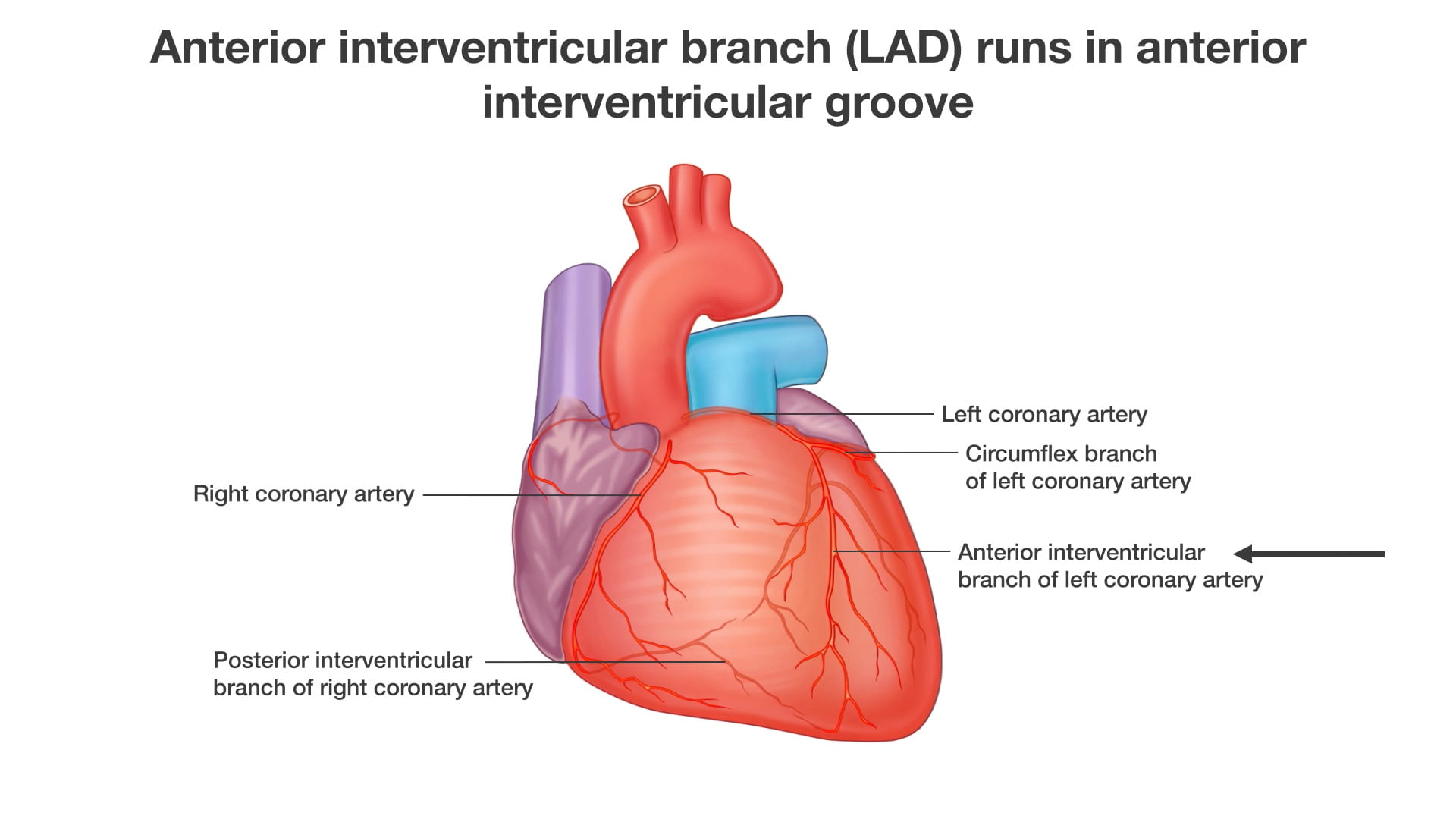
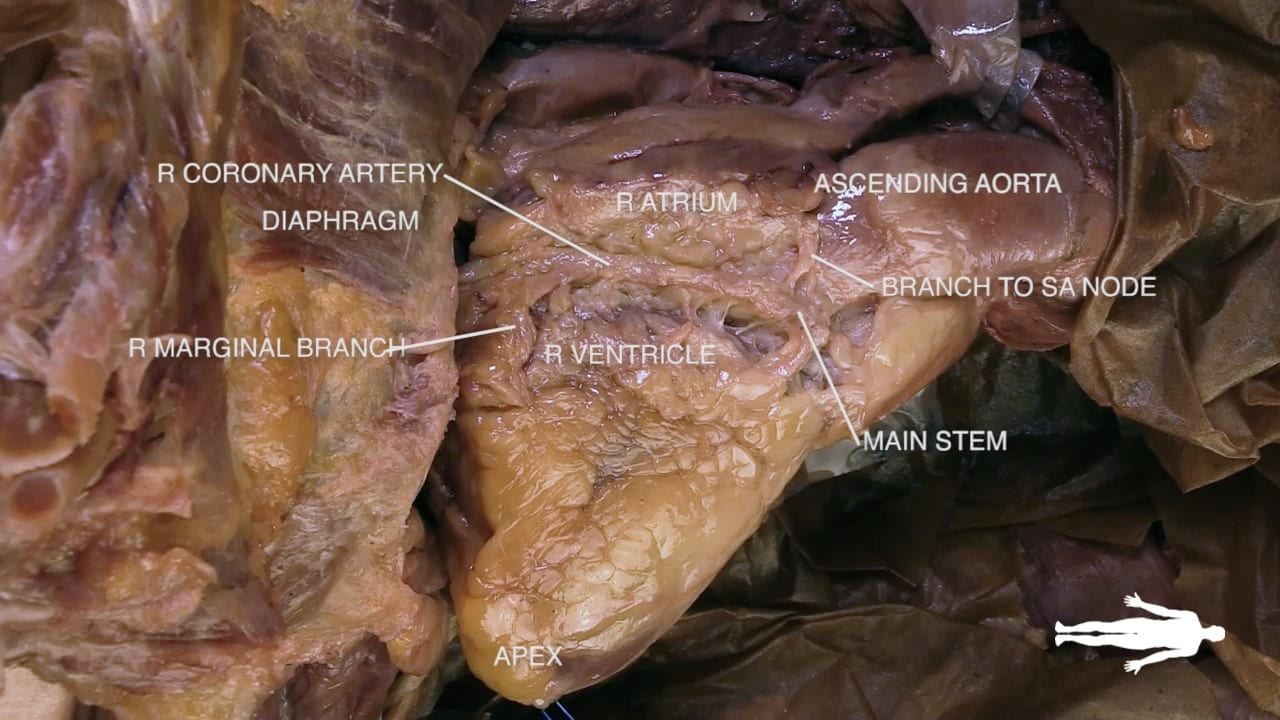
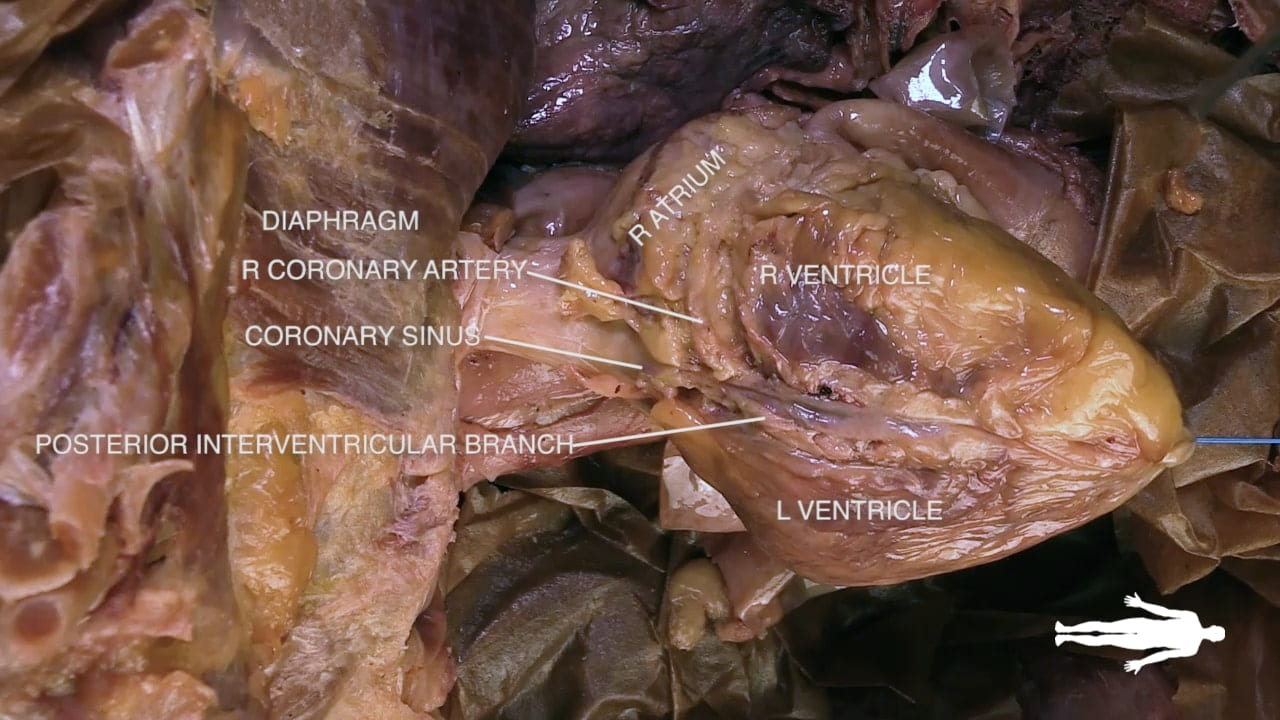
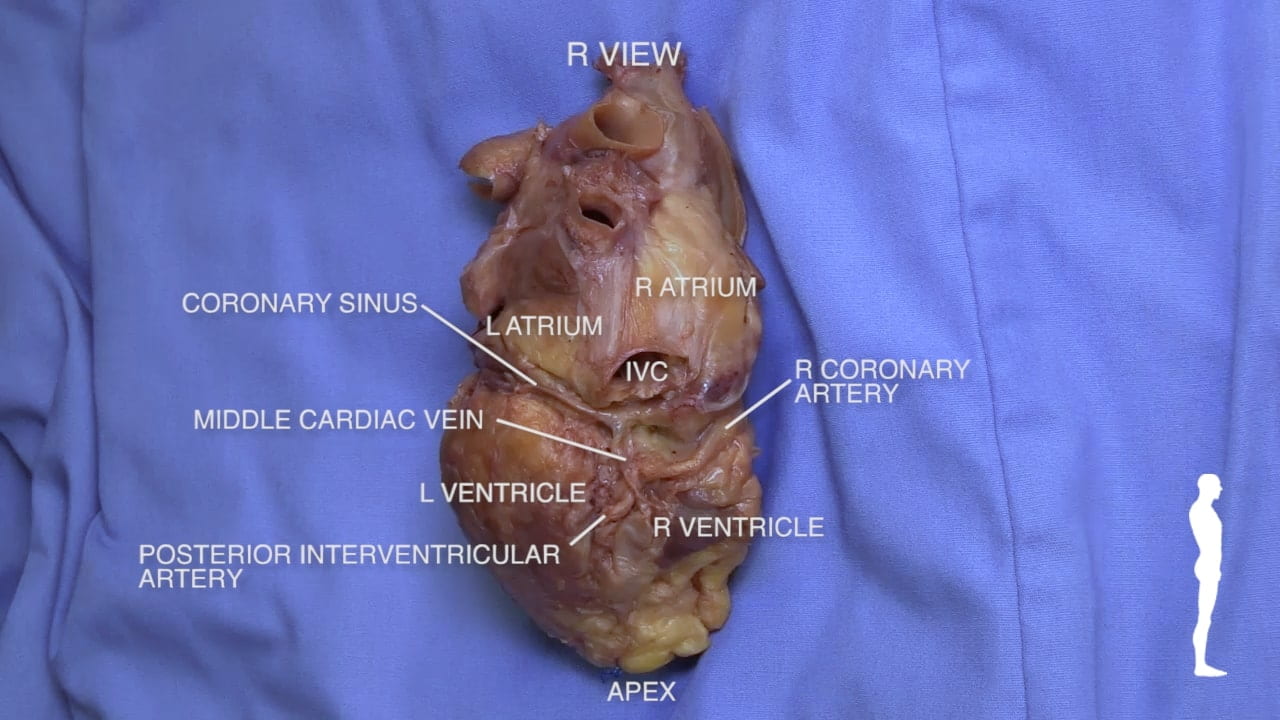
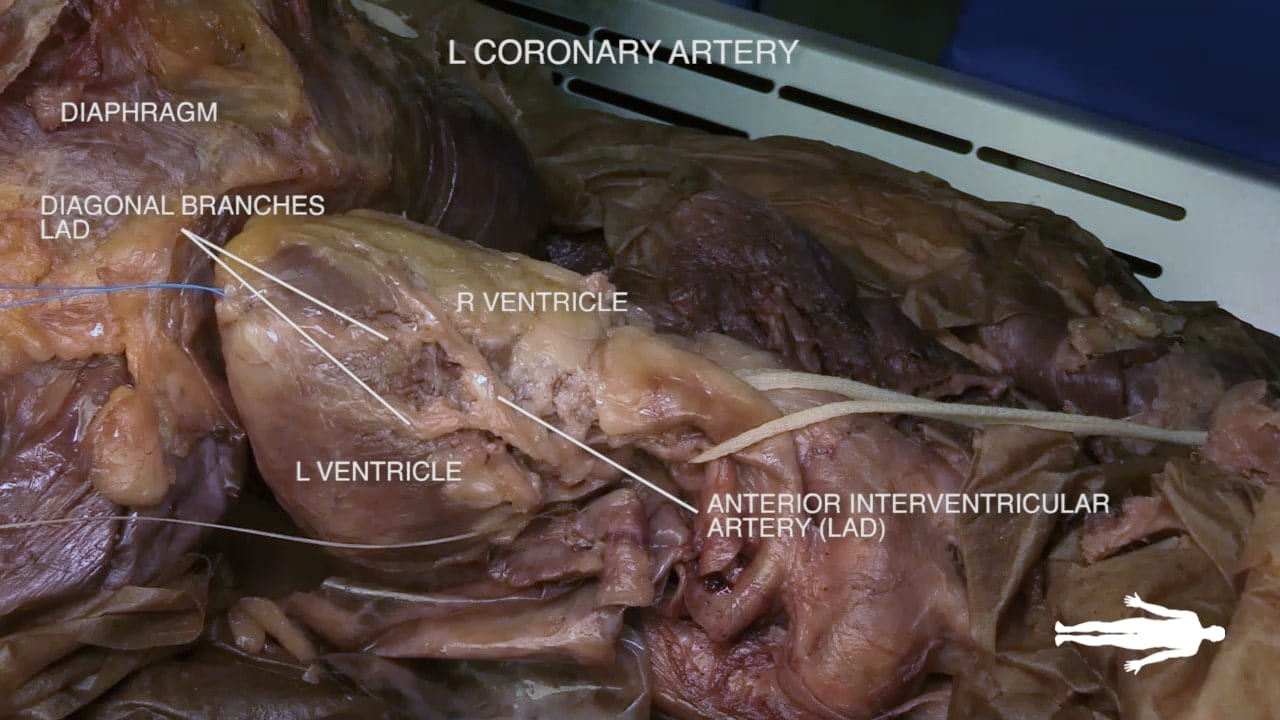
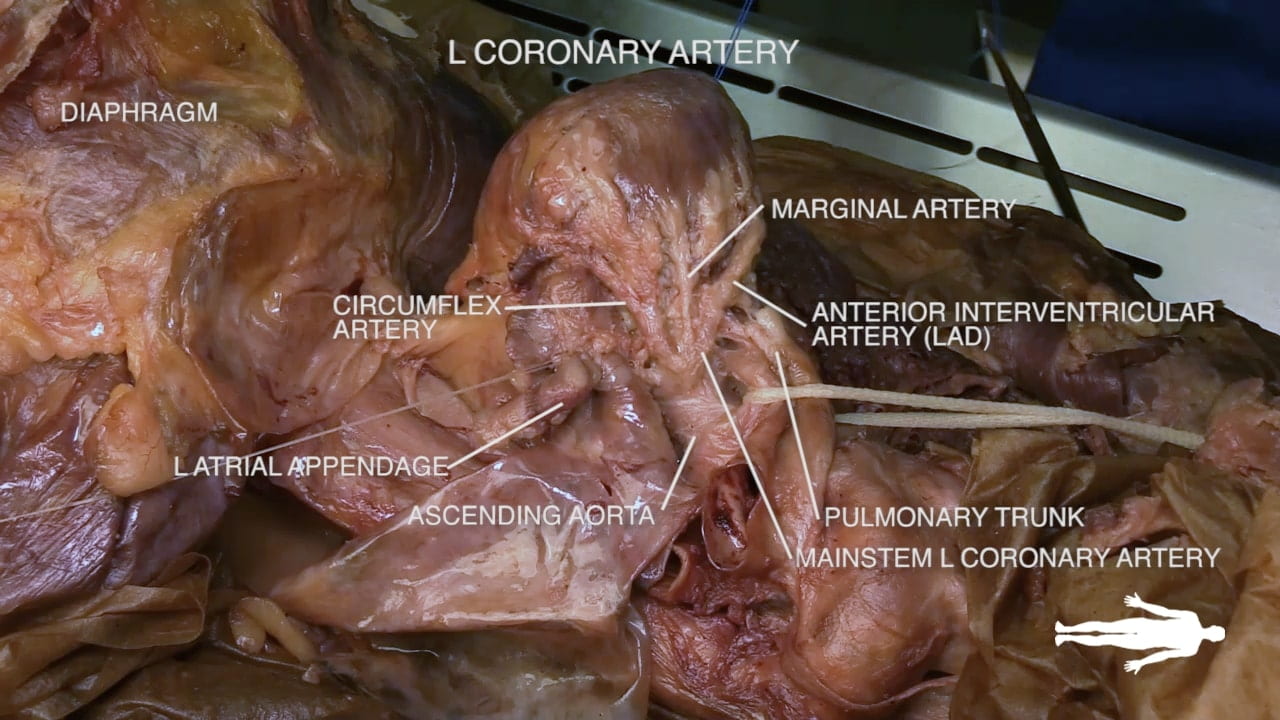
- Describe the location of the major branches of the coronary arteries in relation to the atrioventricular and interventricular grooves.
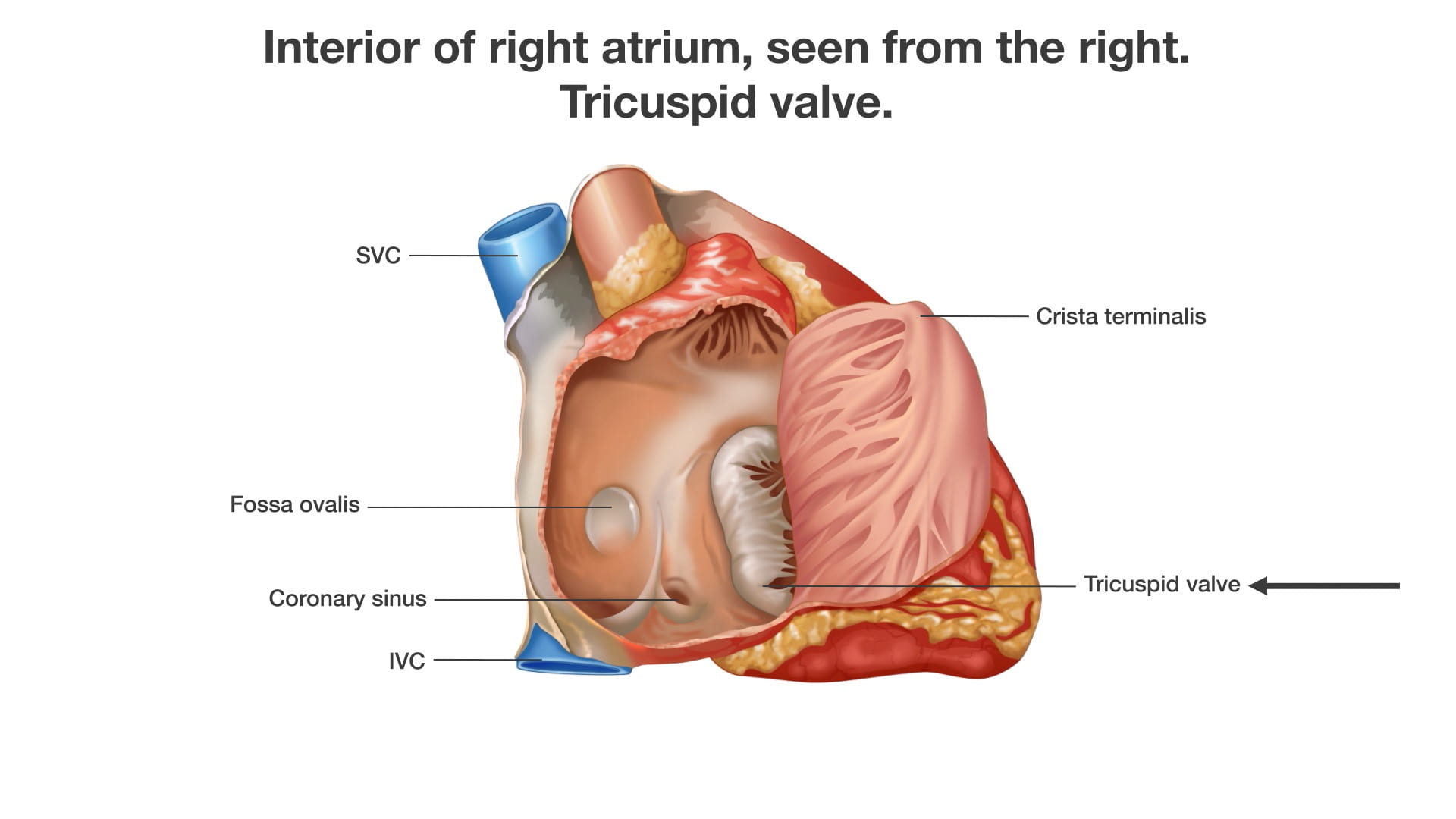
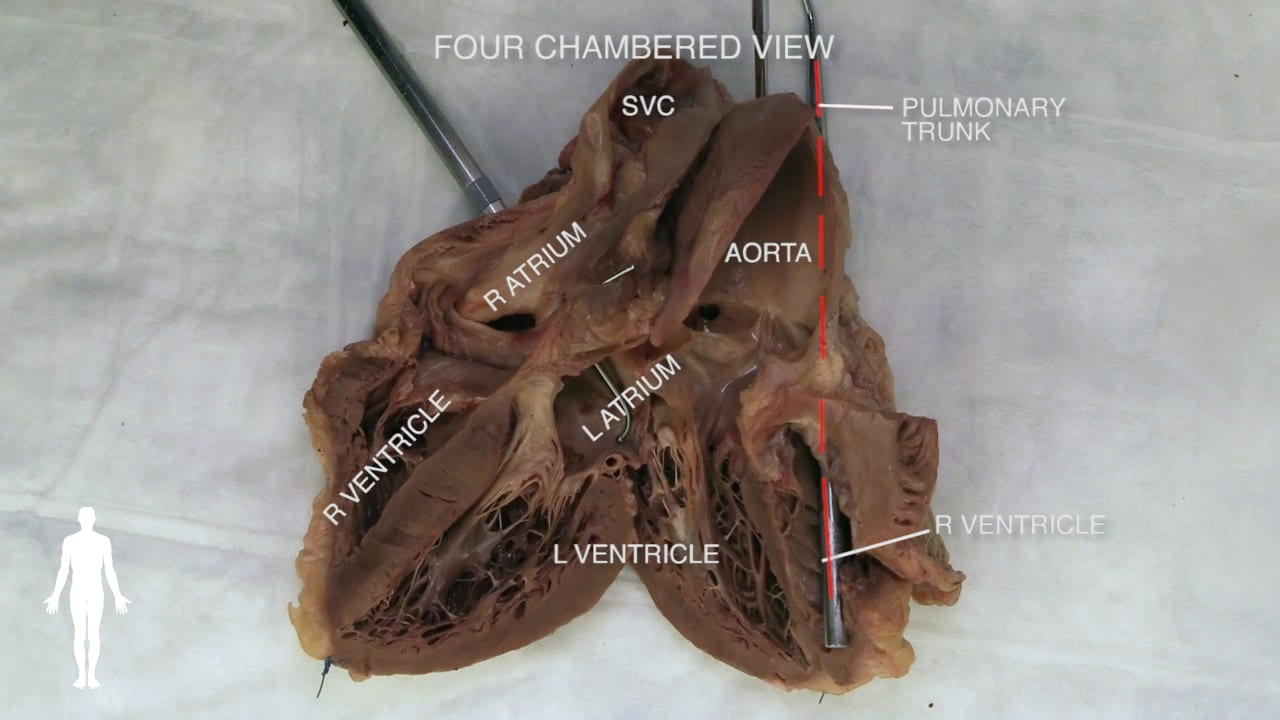
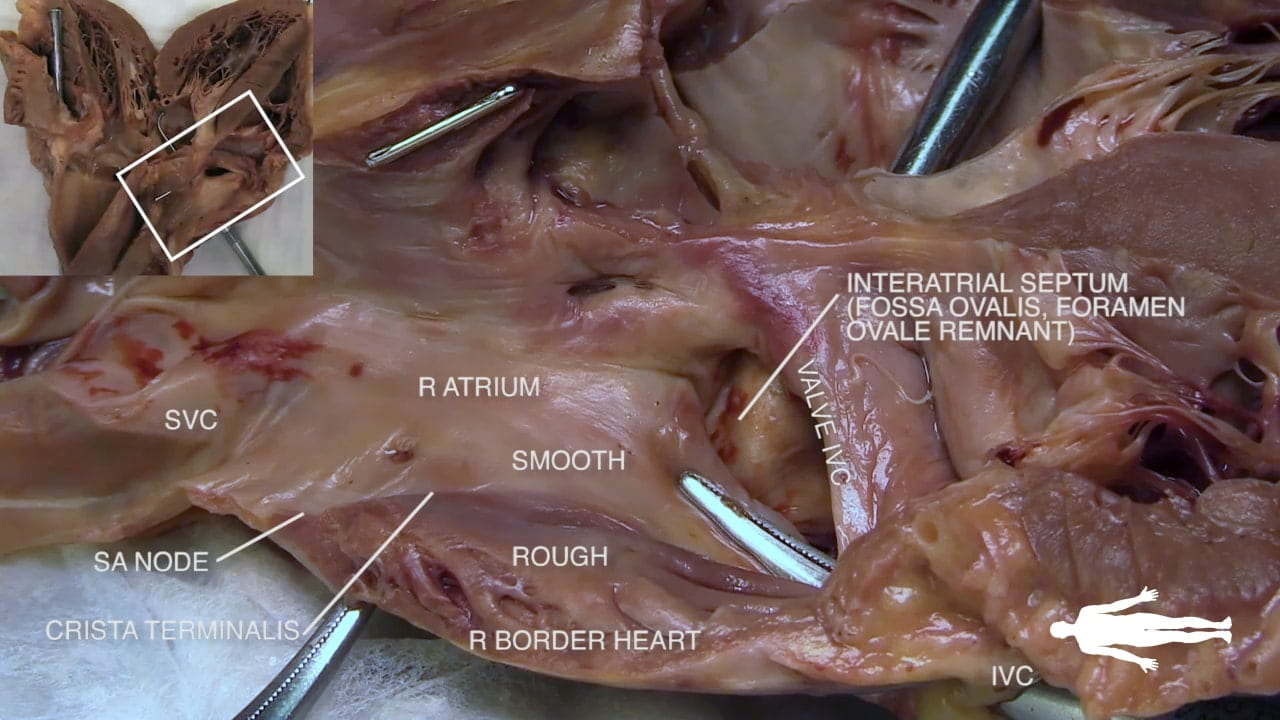
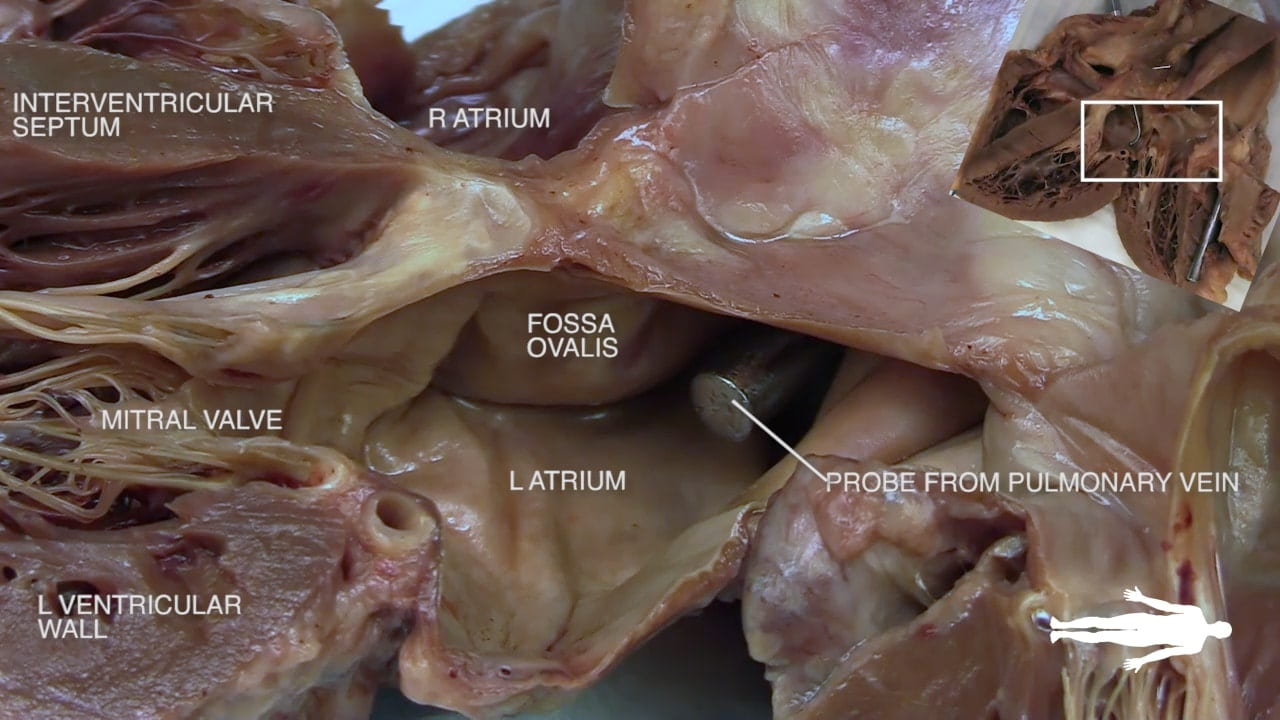
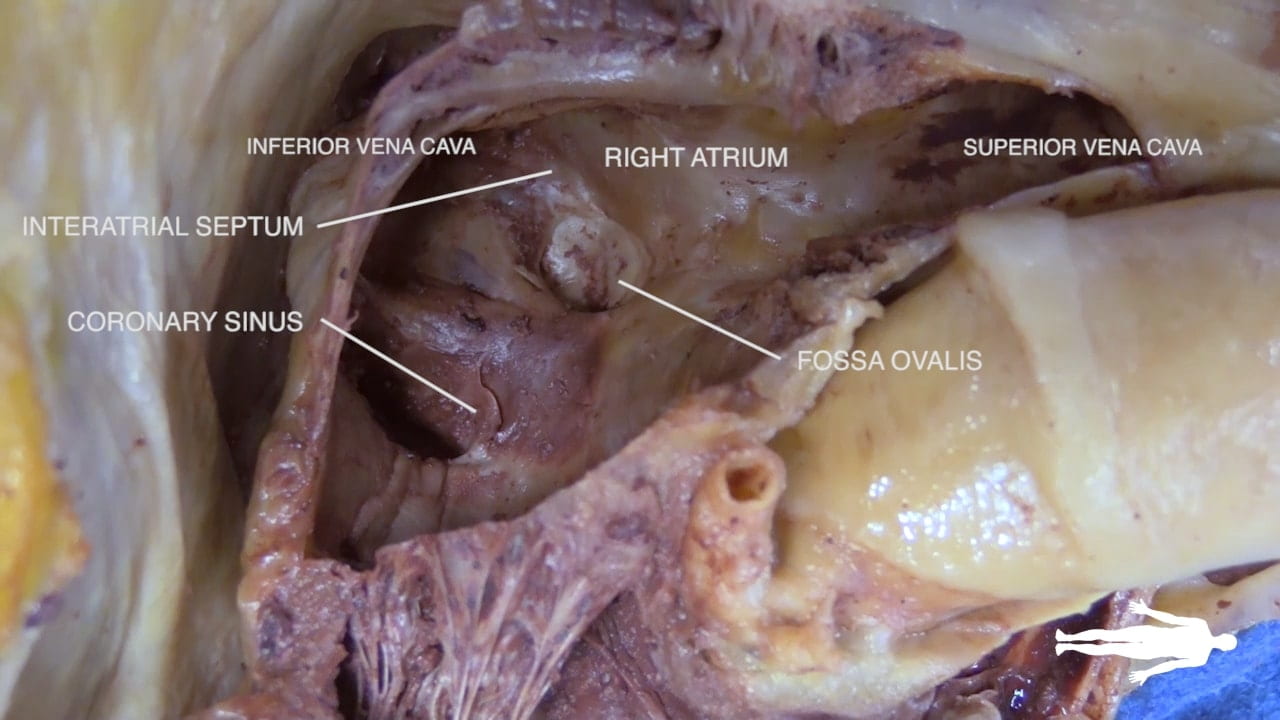
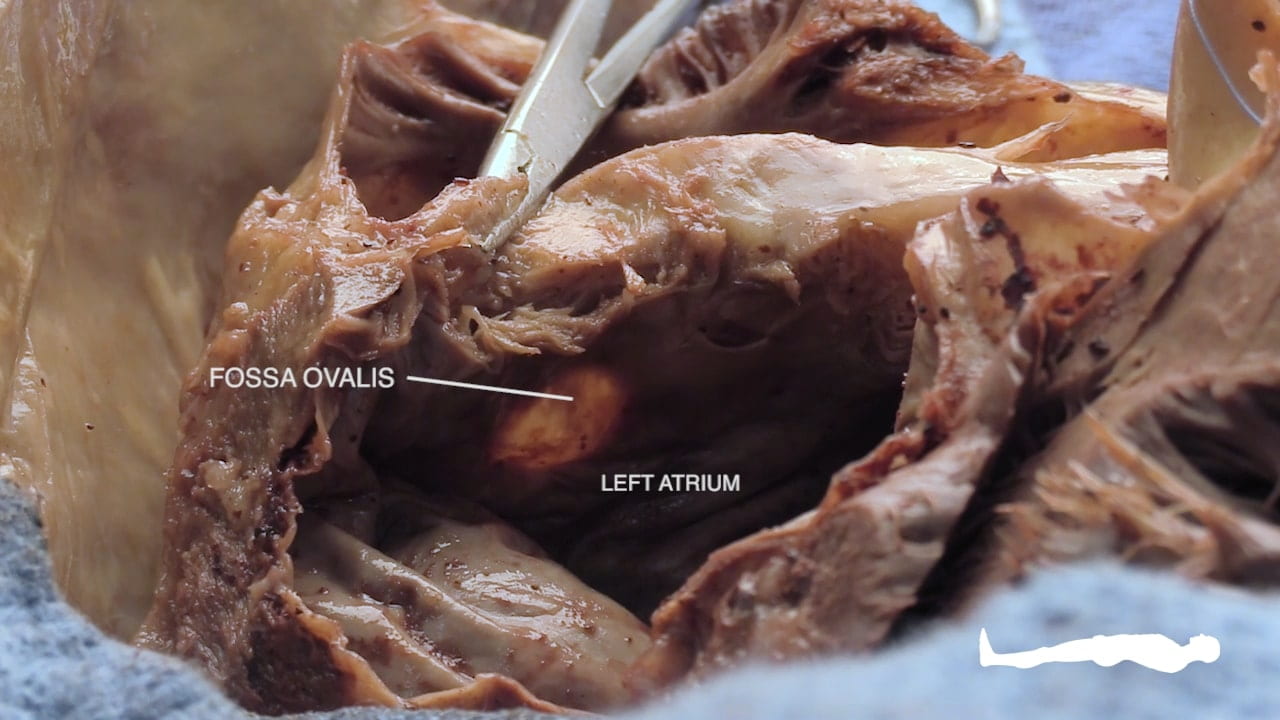
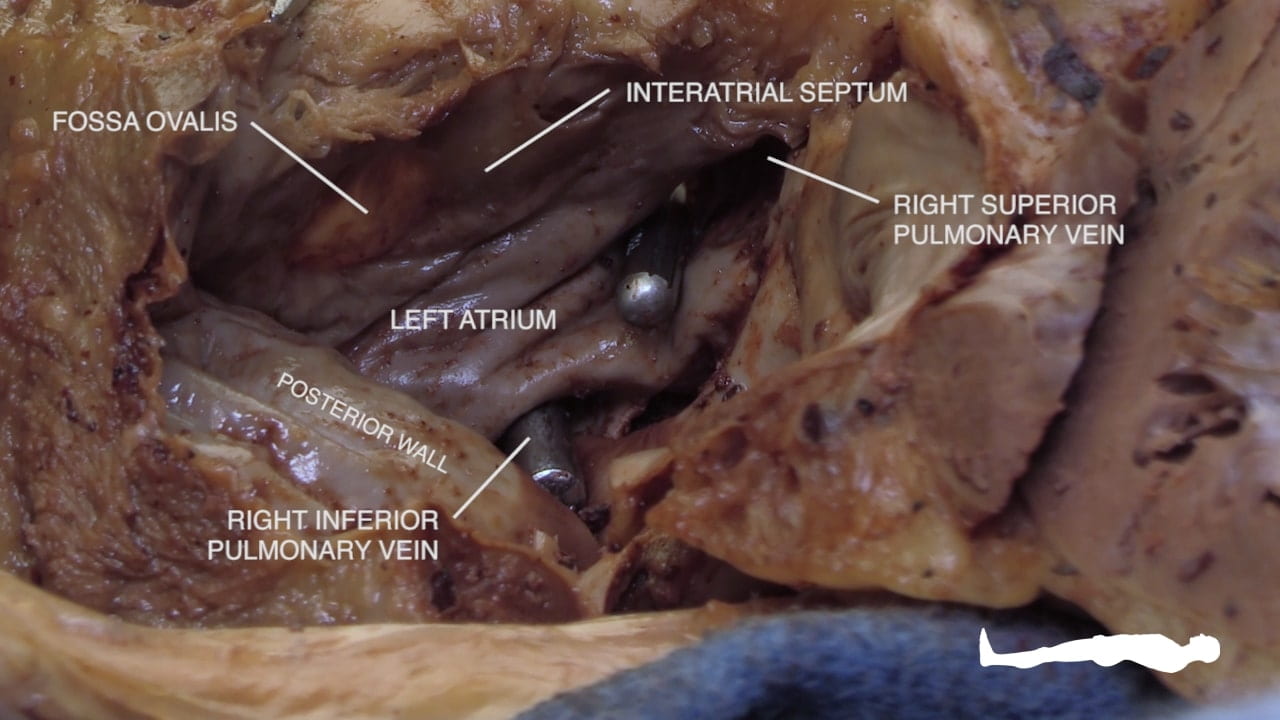
- Describe the position and significance of the ligamentum arteriosum and fossa ovalis.
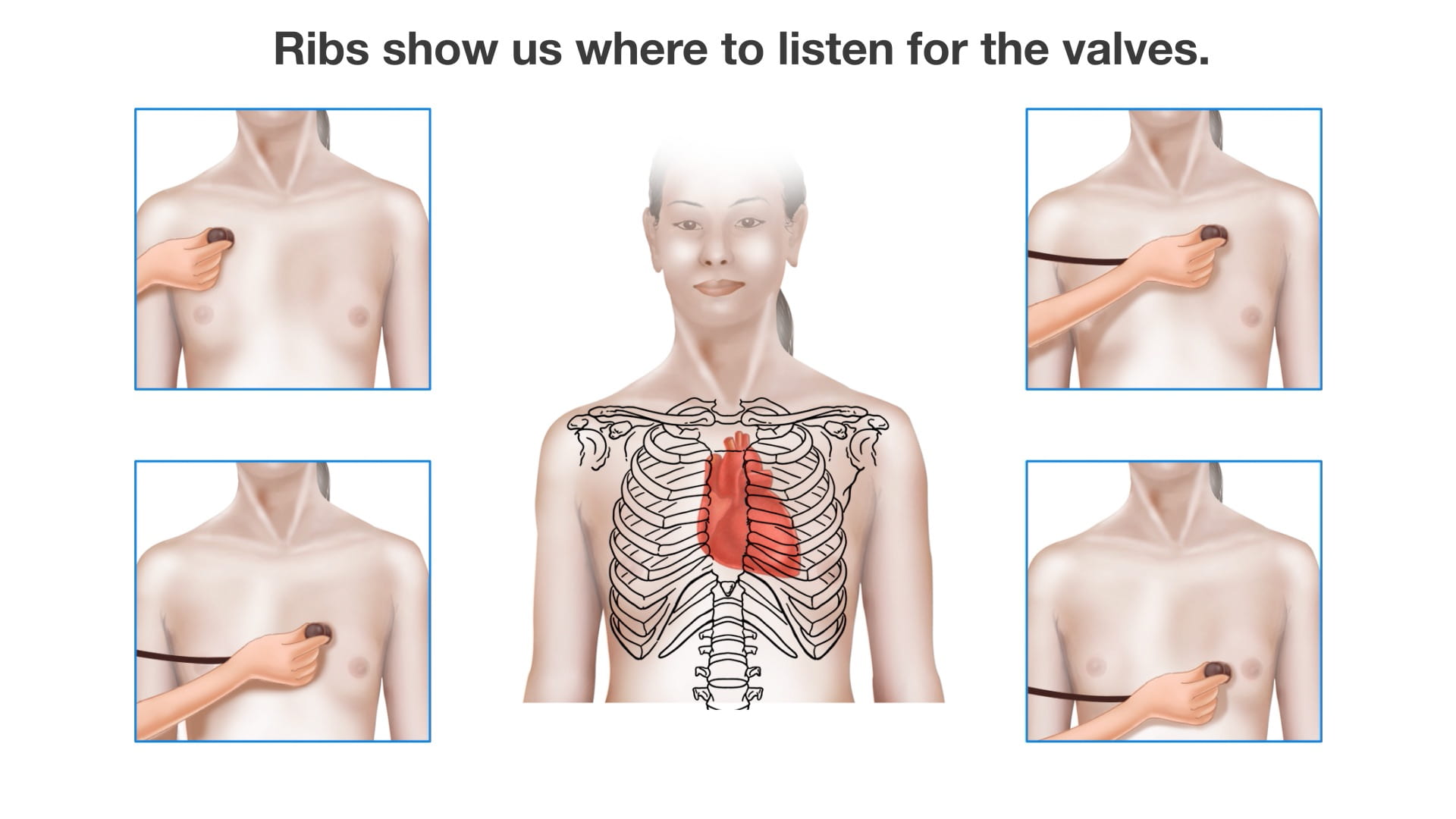
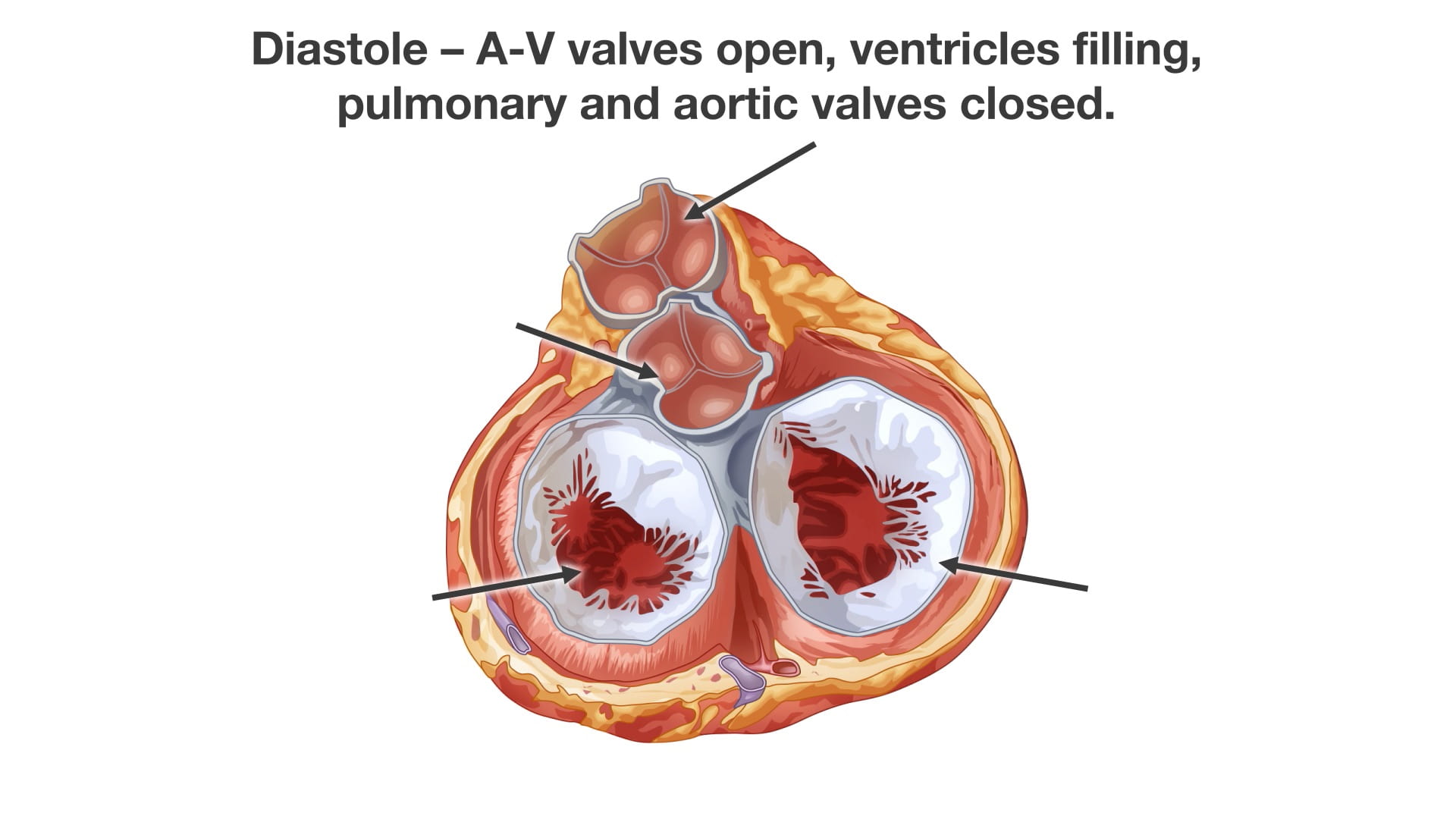
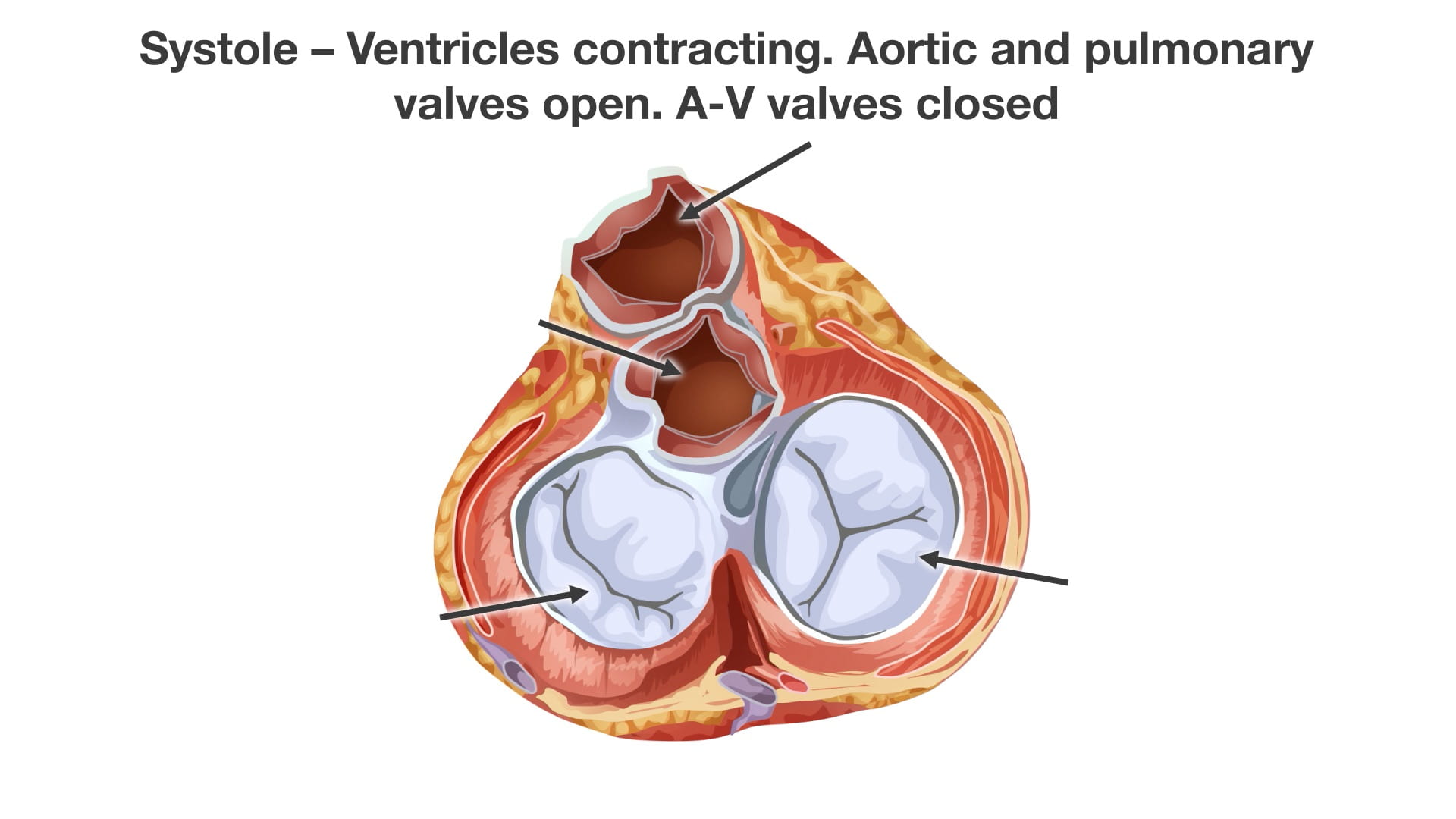
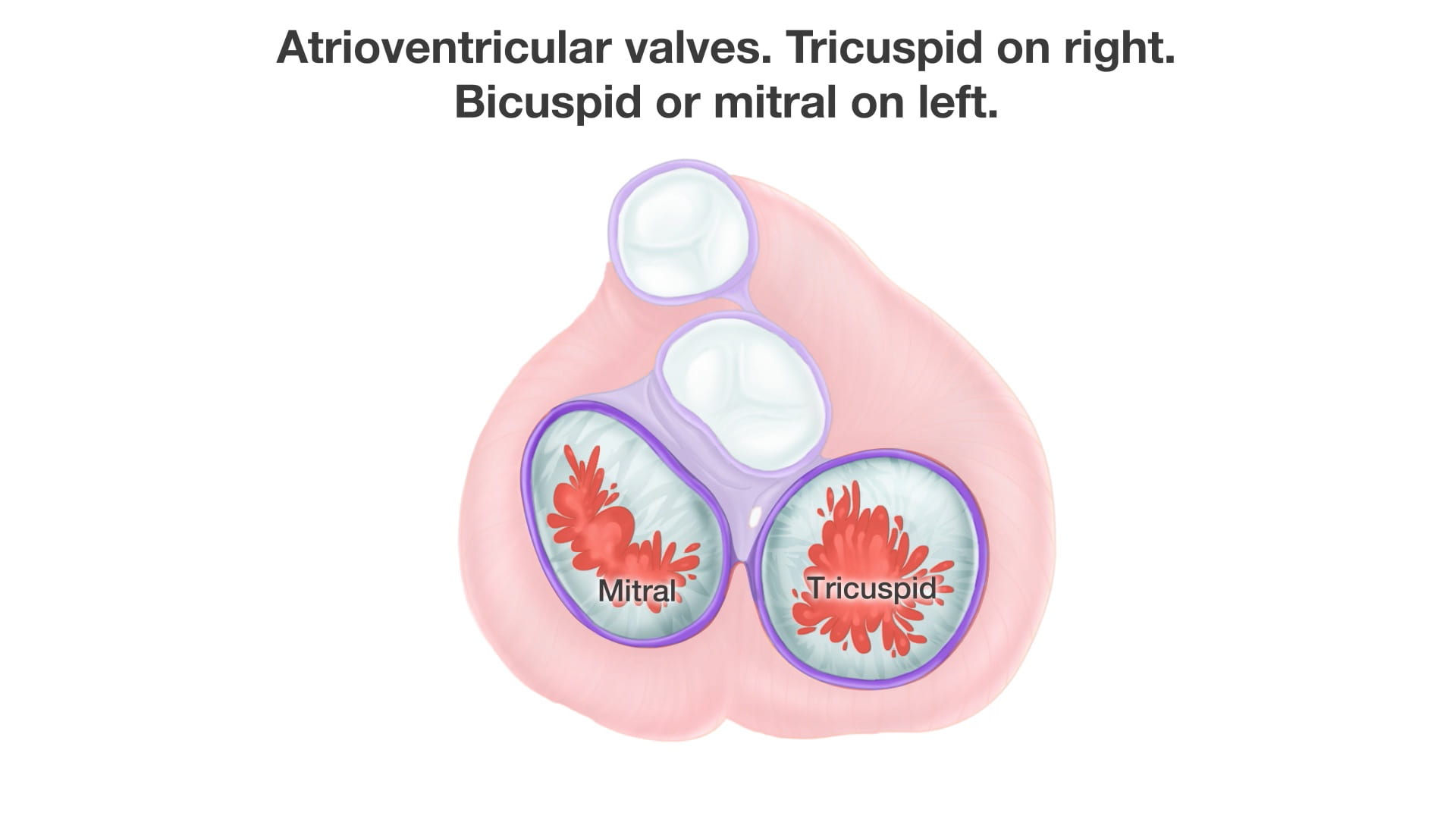
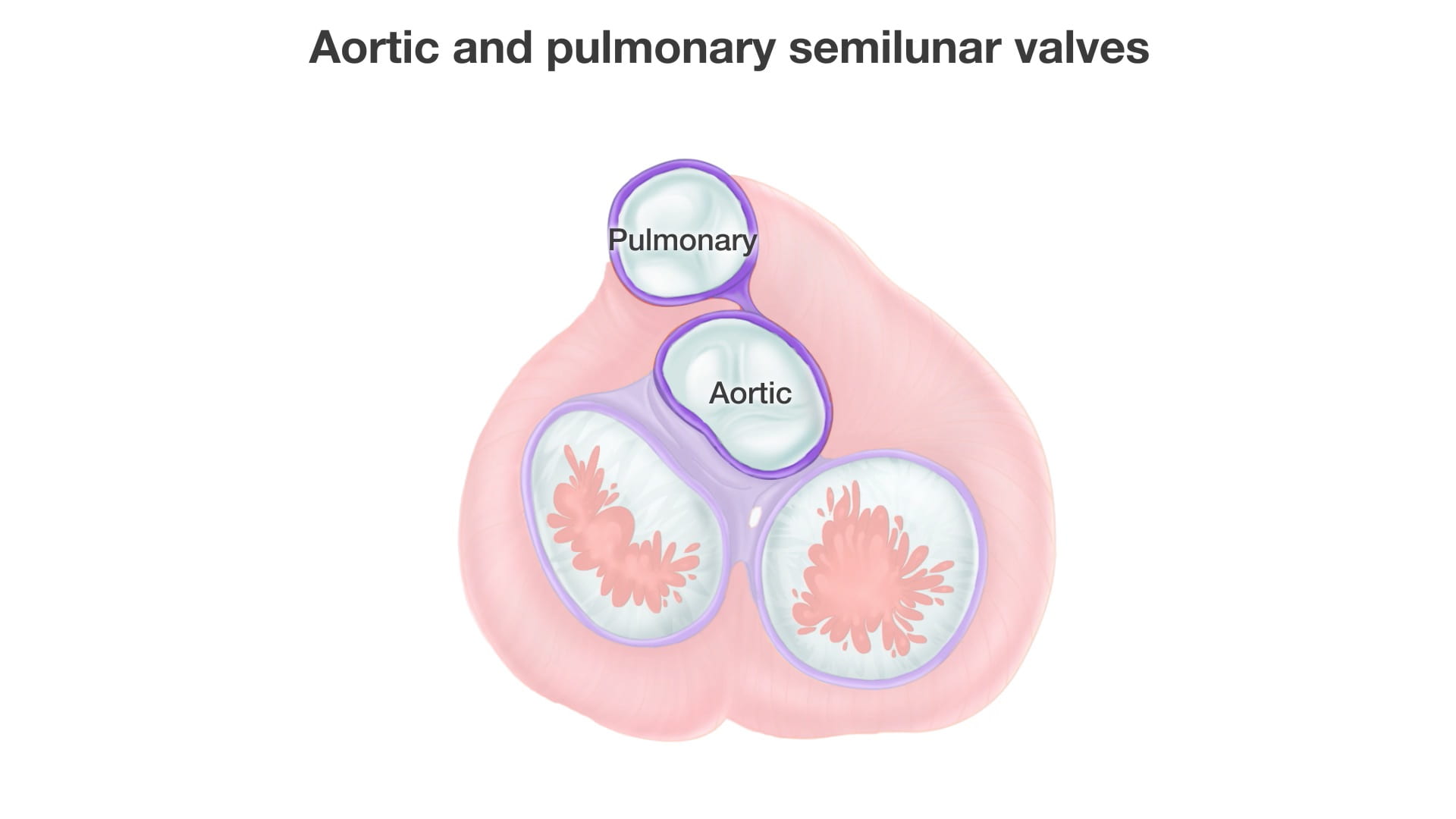
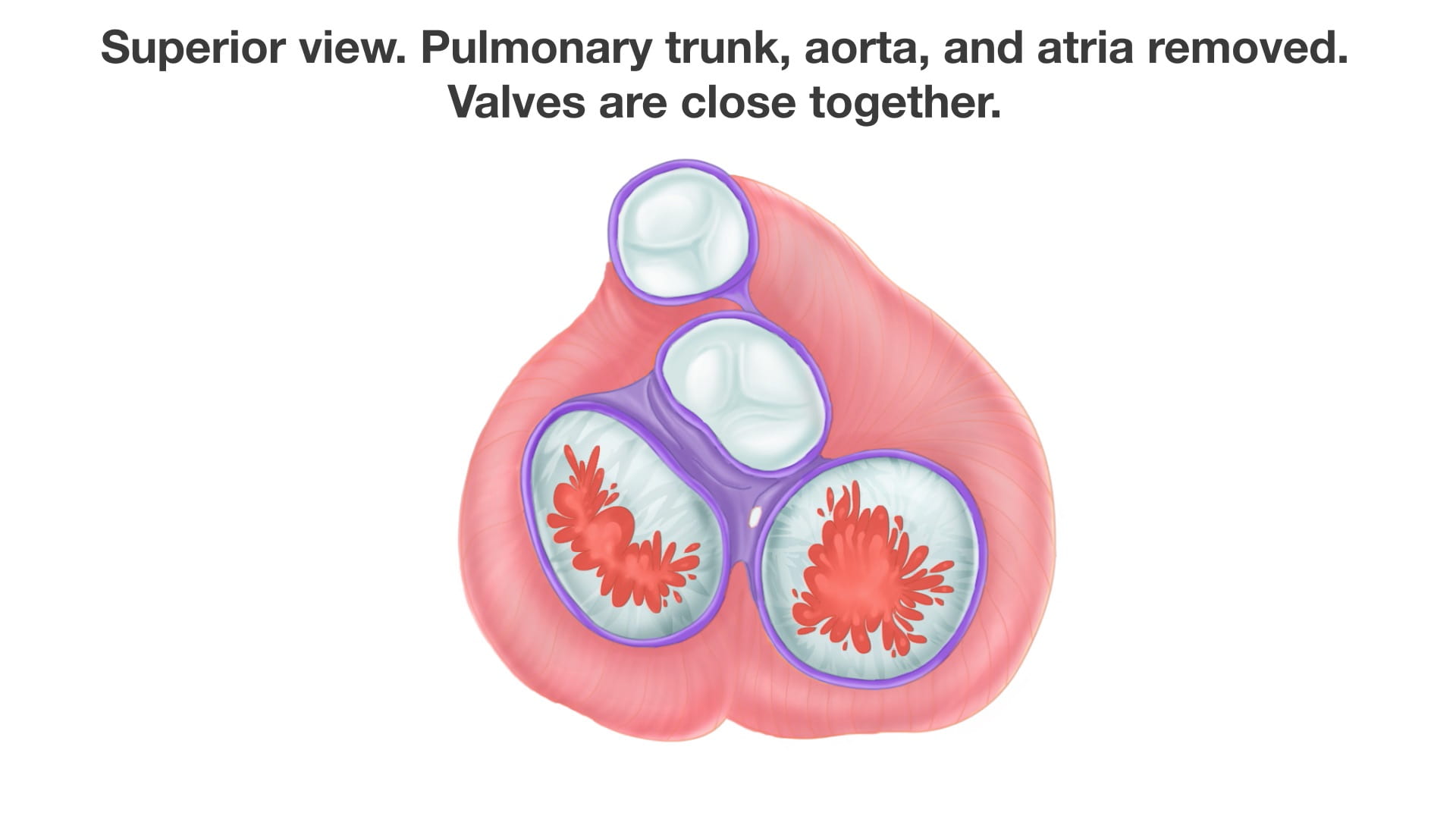
- Name the valves of the heart and the chambers / vessels they connect.
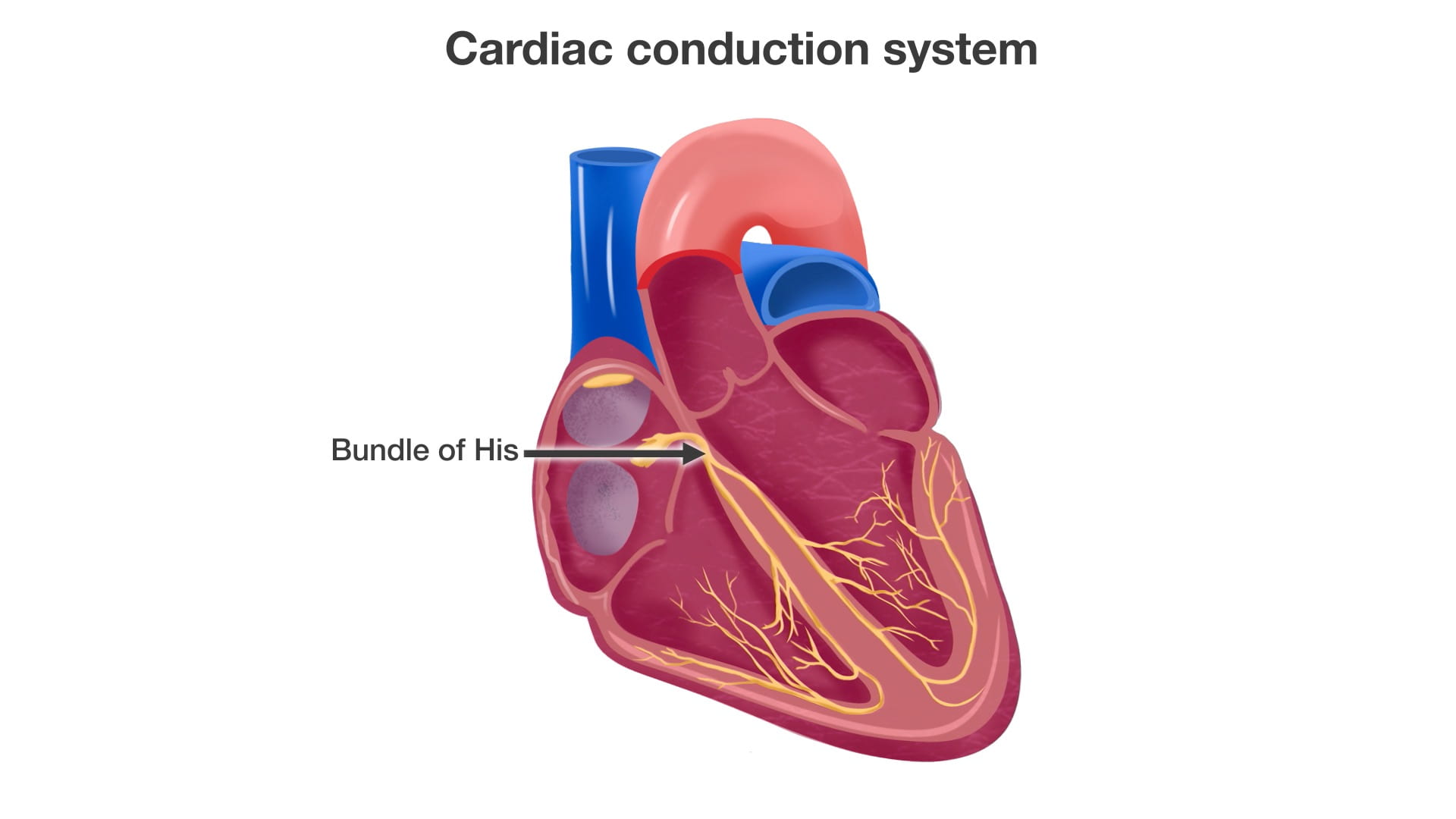
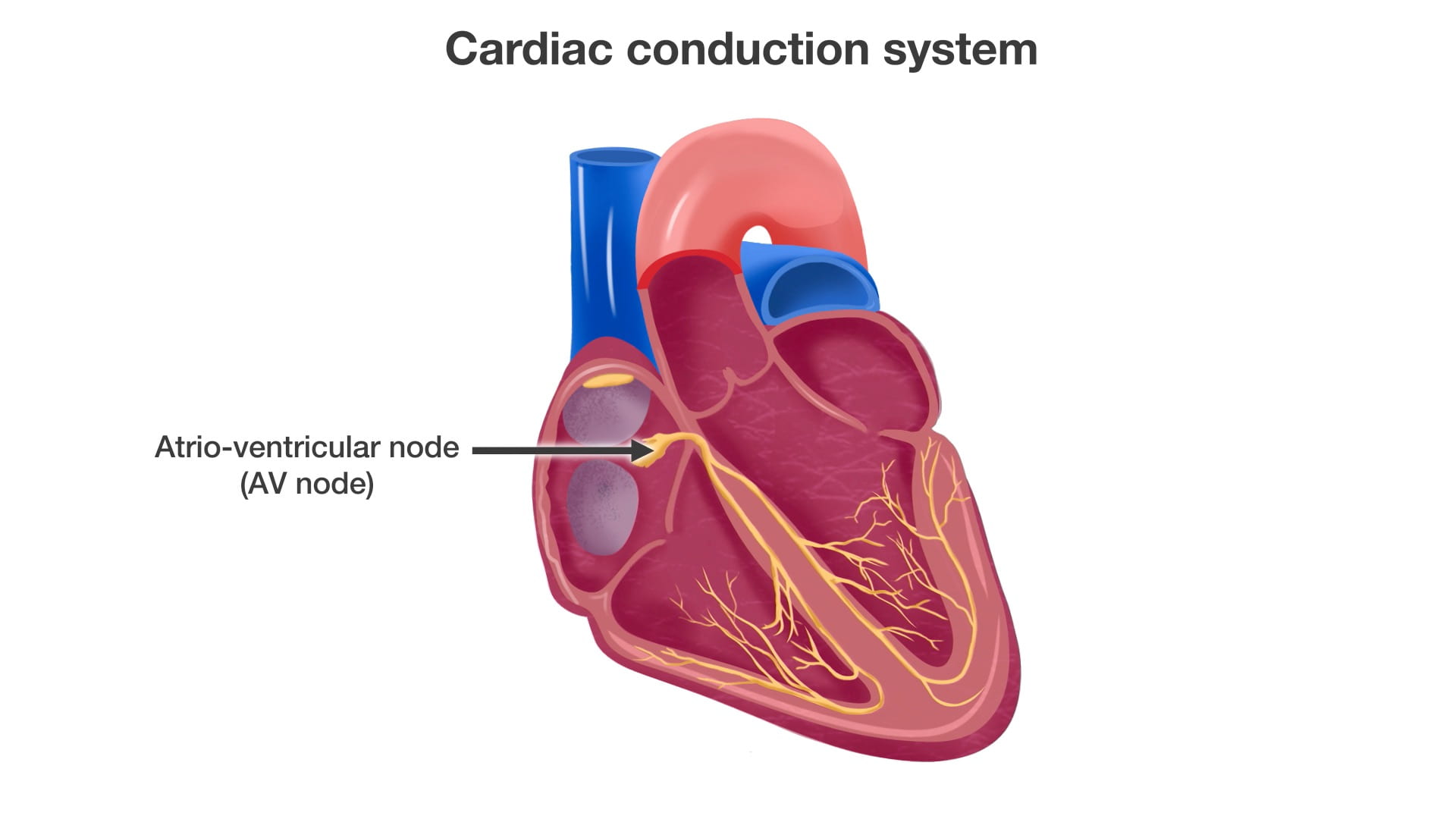
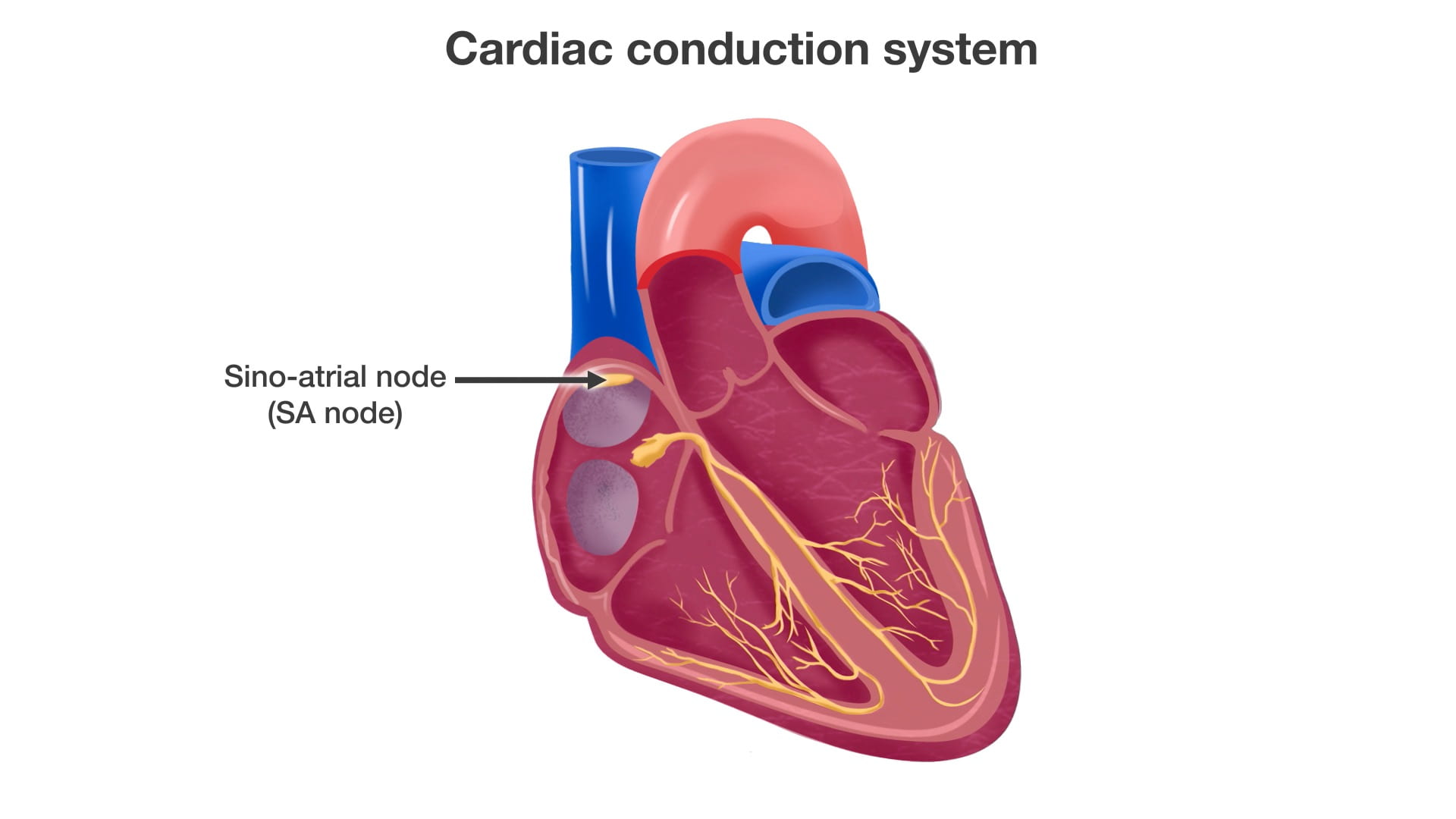
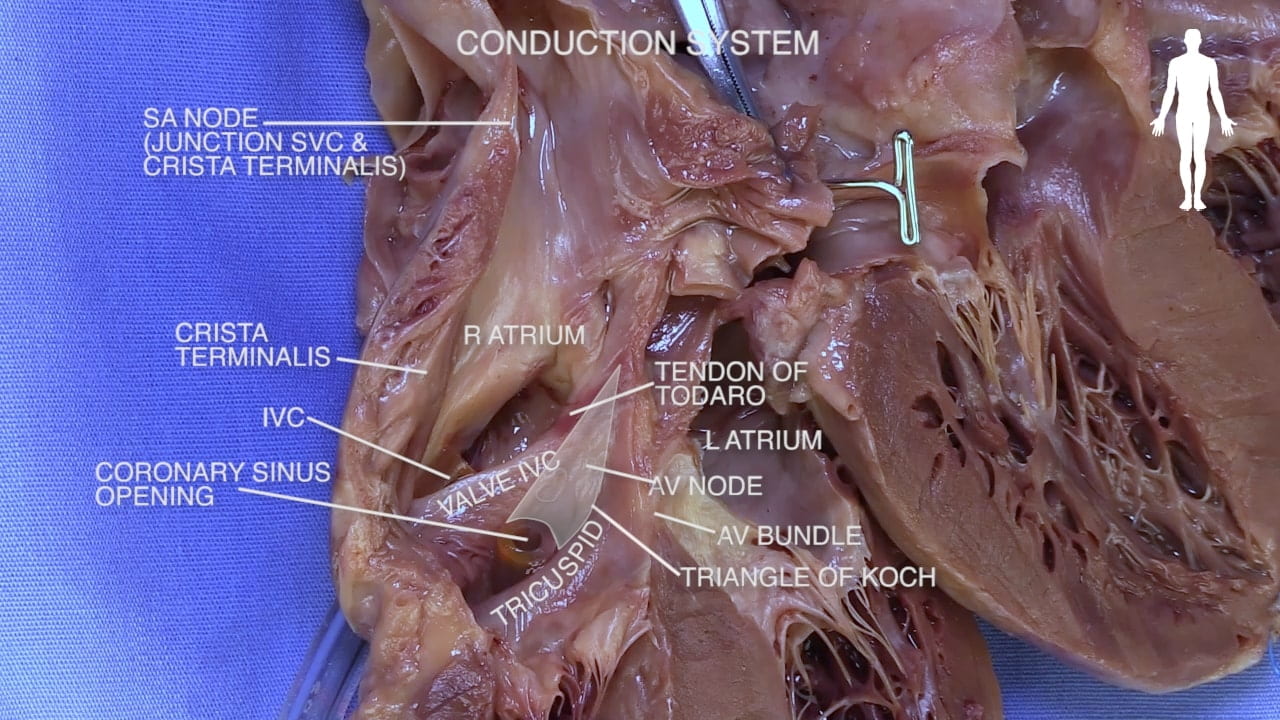
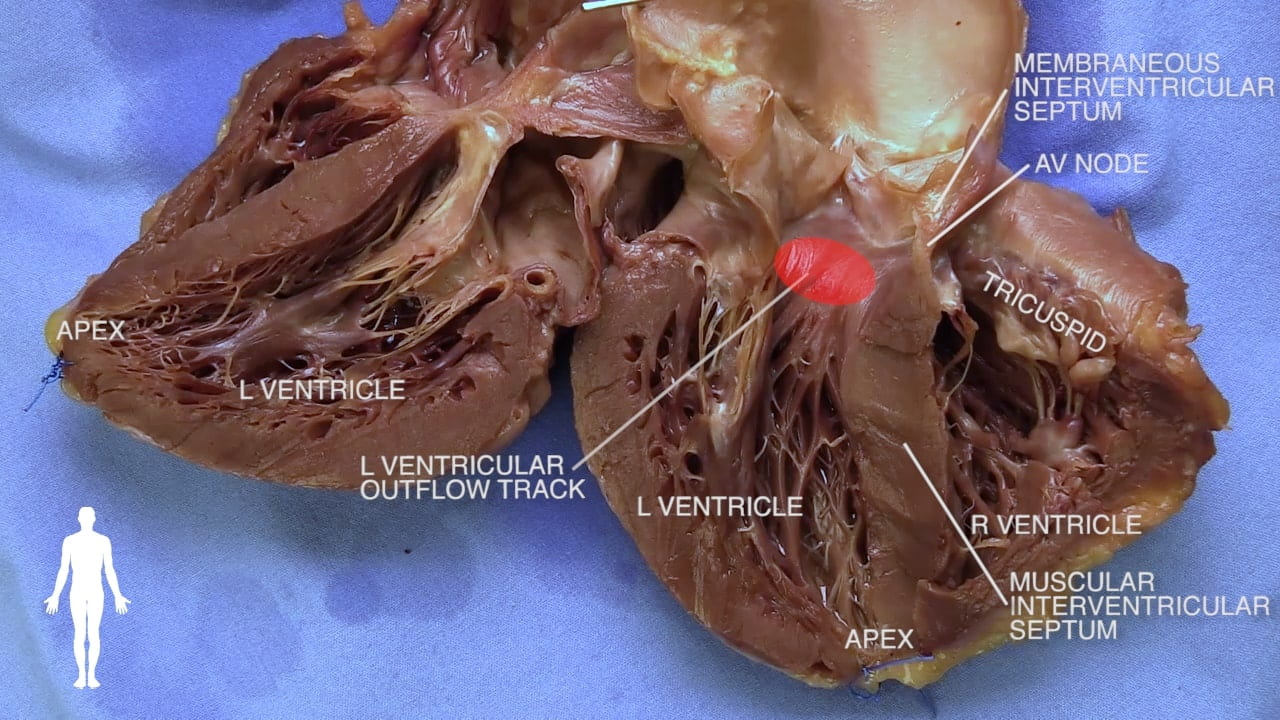
- Describe the approximate location of the sinoatrial (SA) and atrioventricular (AV) nodes.
- Describe the conduction system of the heart.
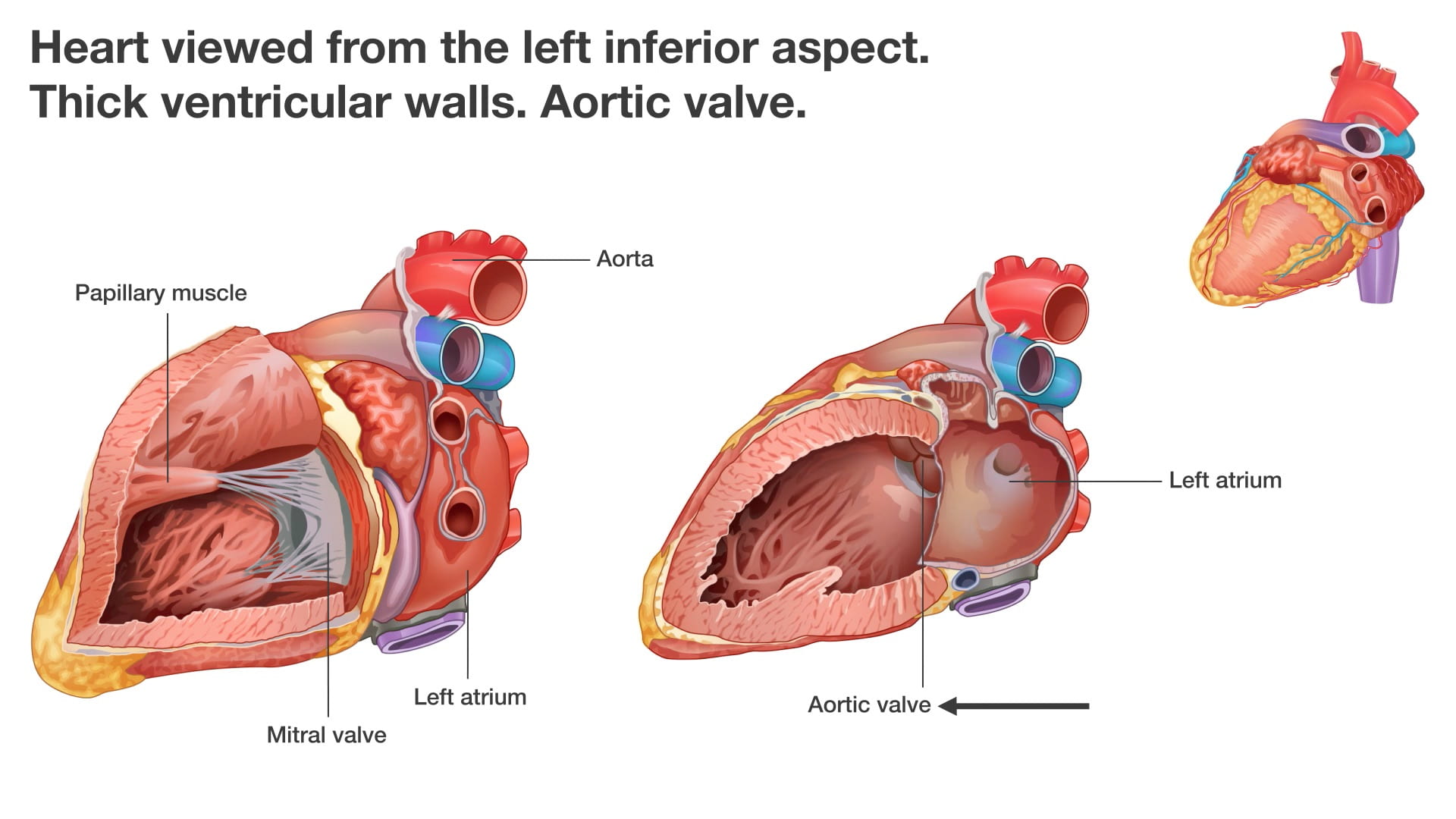
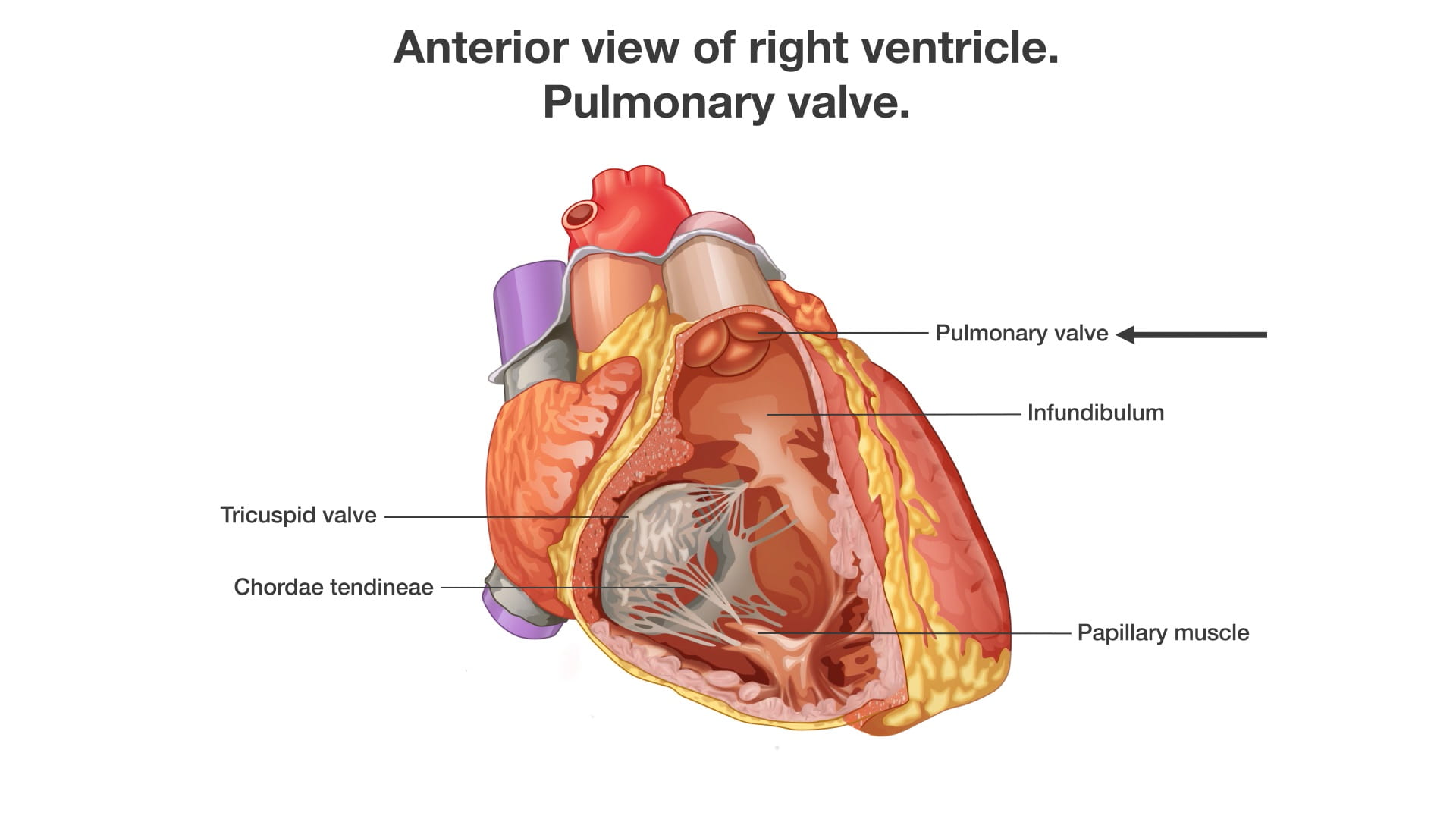
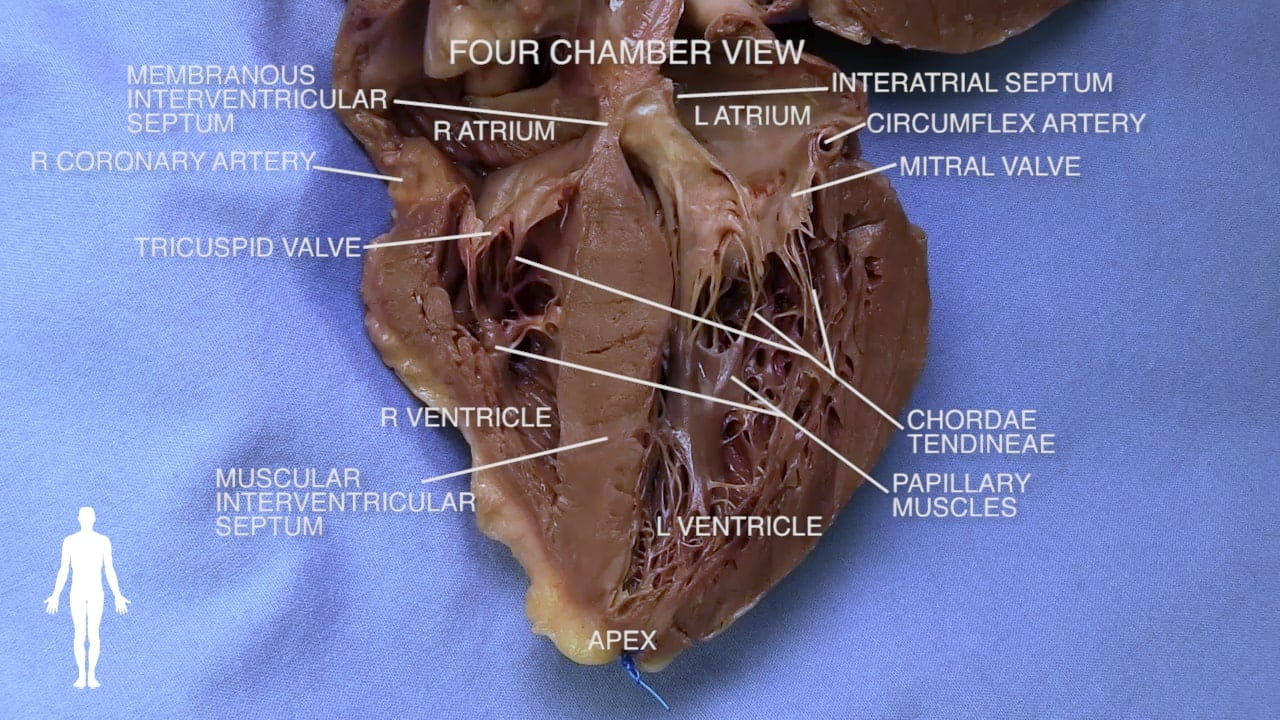
- Describe the functional importance of papillary muscles and chordae tendineae.
Lecture List
The Heart, Exposure of the Heart, Coronary Vessels, Removal of the Heart, Bisecting the Heart, In Situ Dissection of the Heart
Anatomy of the Heart
The Heart Gallery
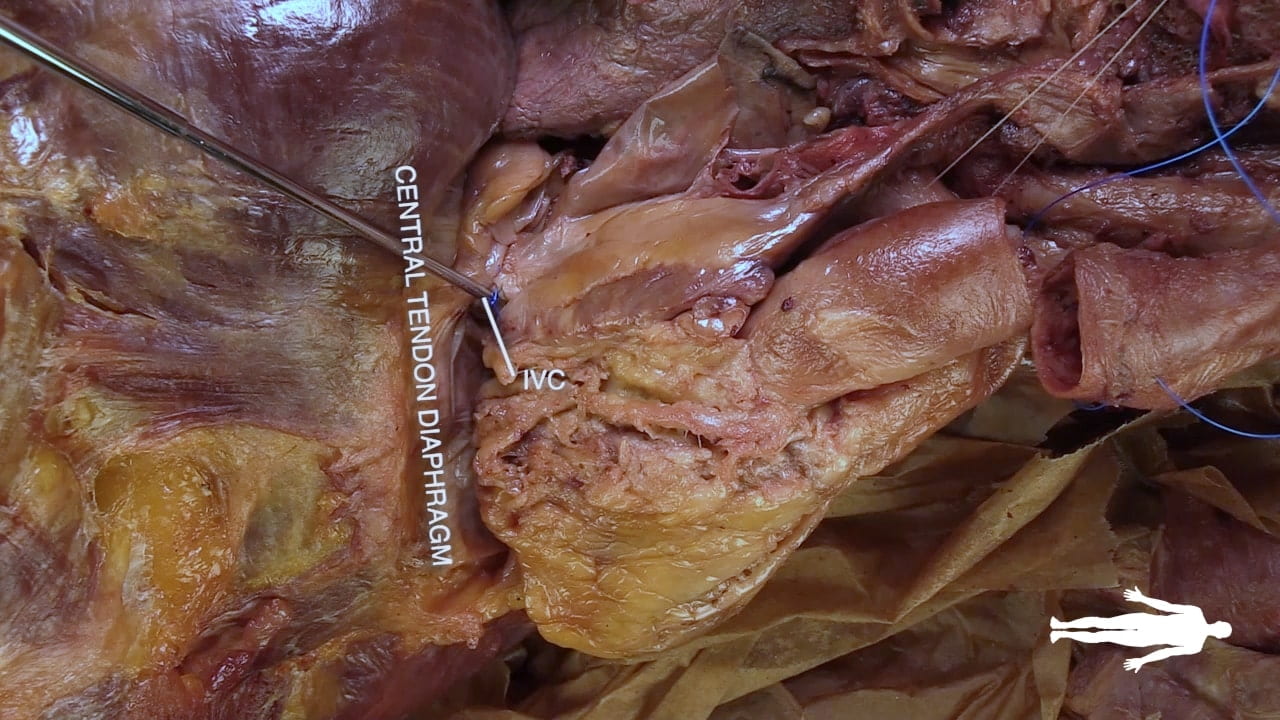
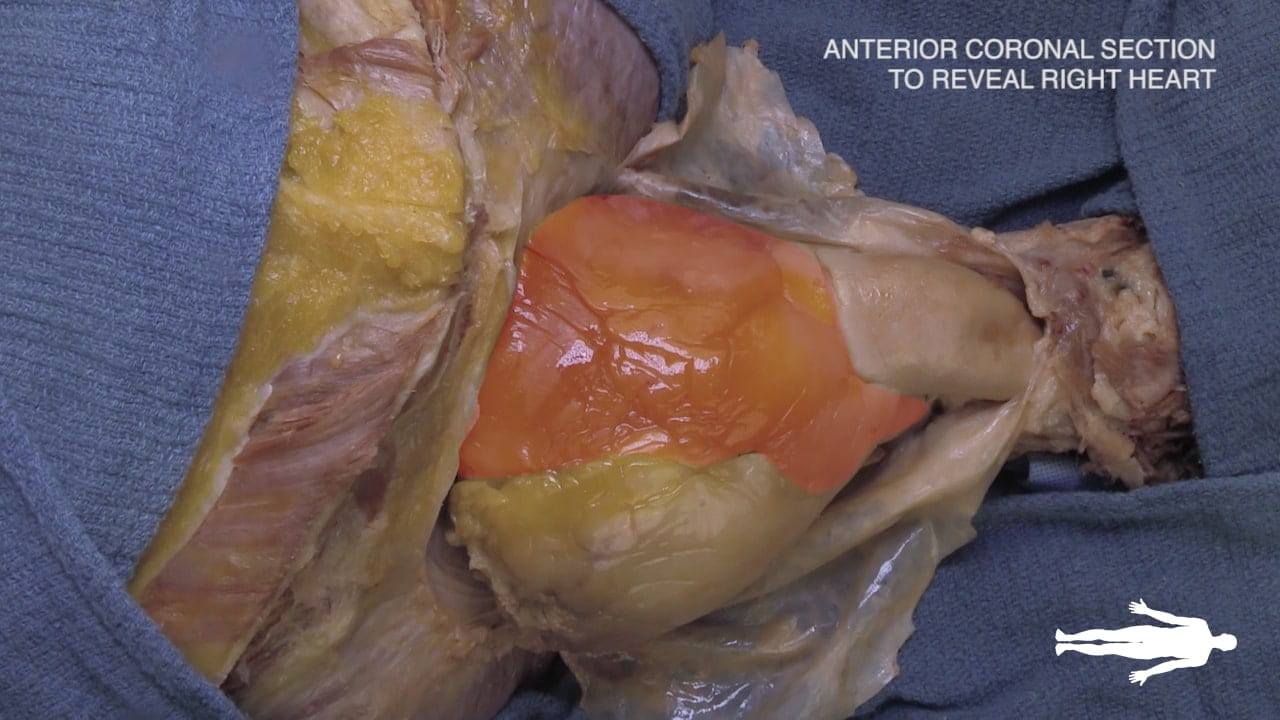
Exposure of Heart
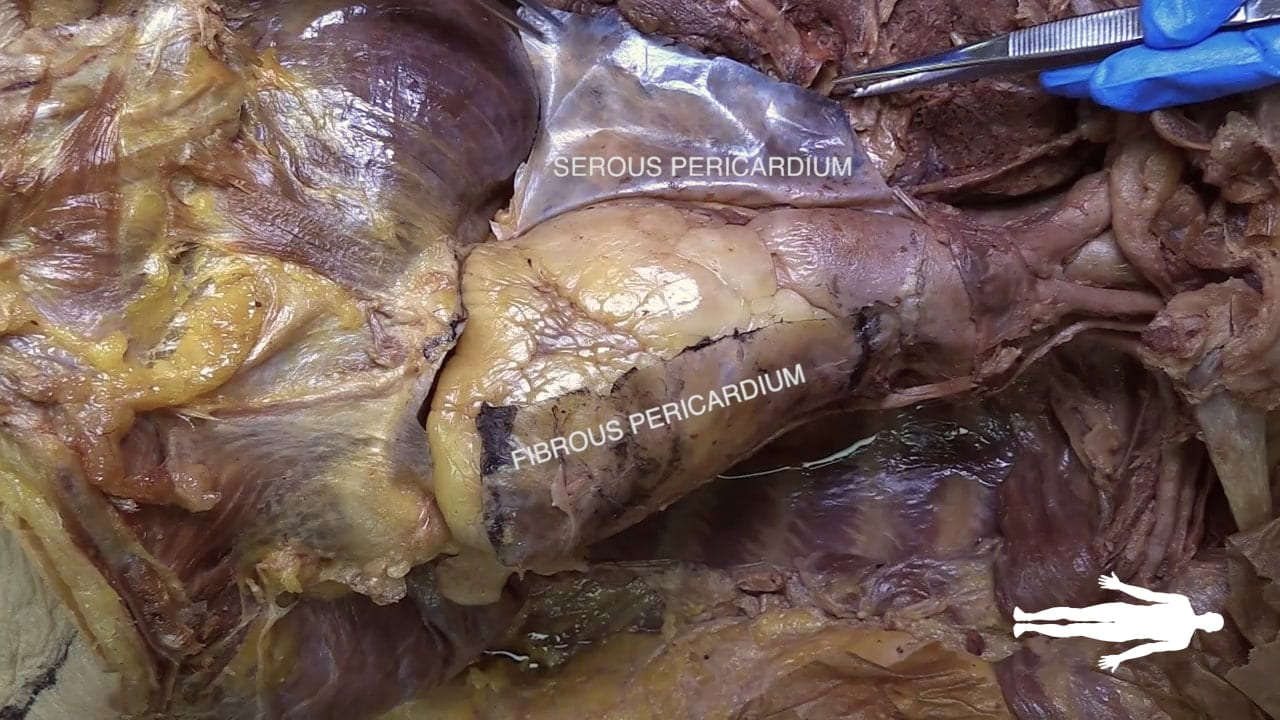
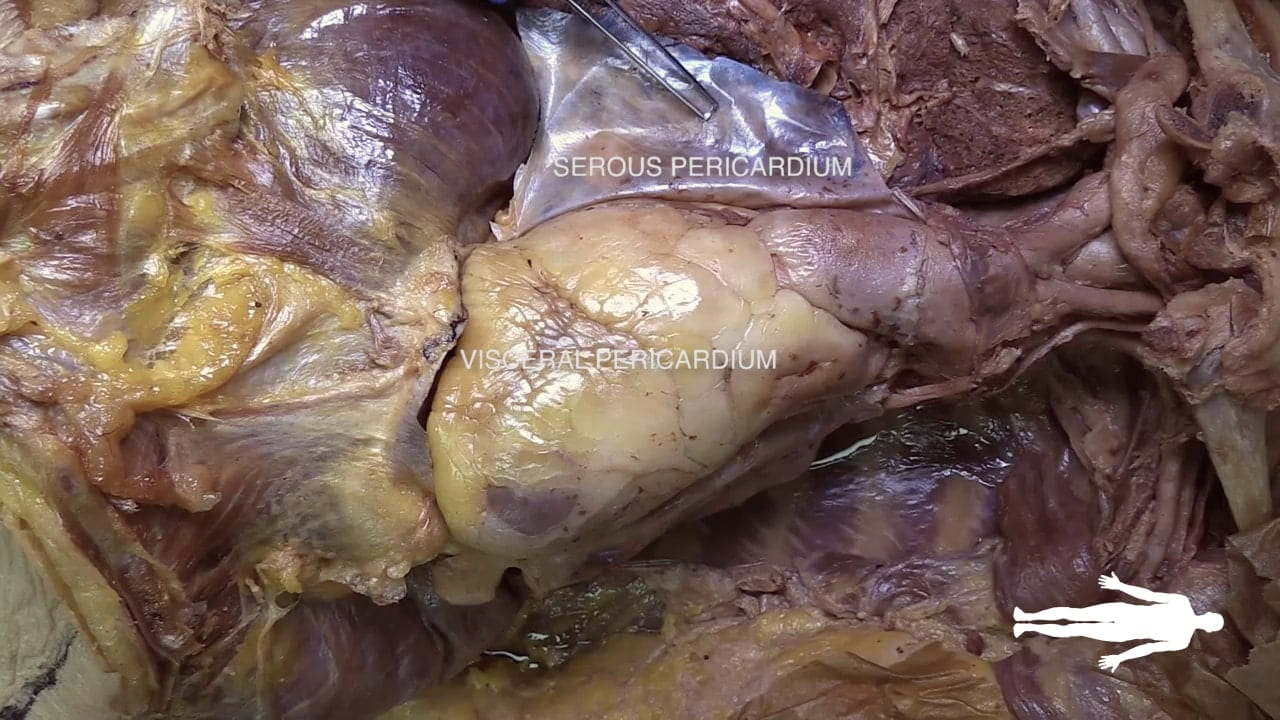
Pericardium
Incise the pericardium in the anterior midline. Open further with transverse incisions at the apex and base.
Identify the fibrous pericardium and the parietal and visceral (epicardium) layers of the serous pericardium.
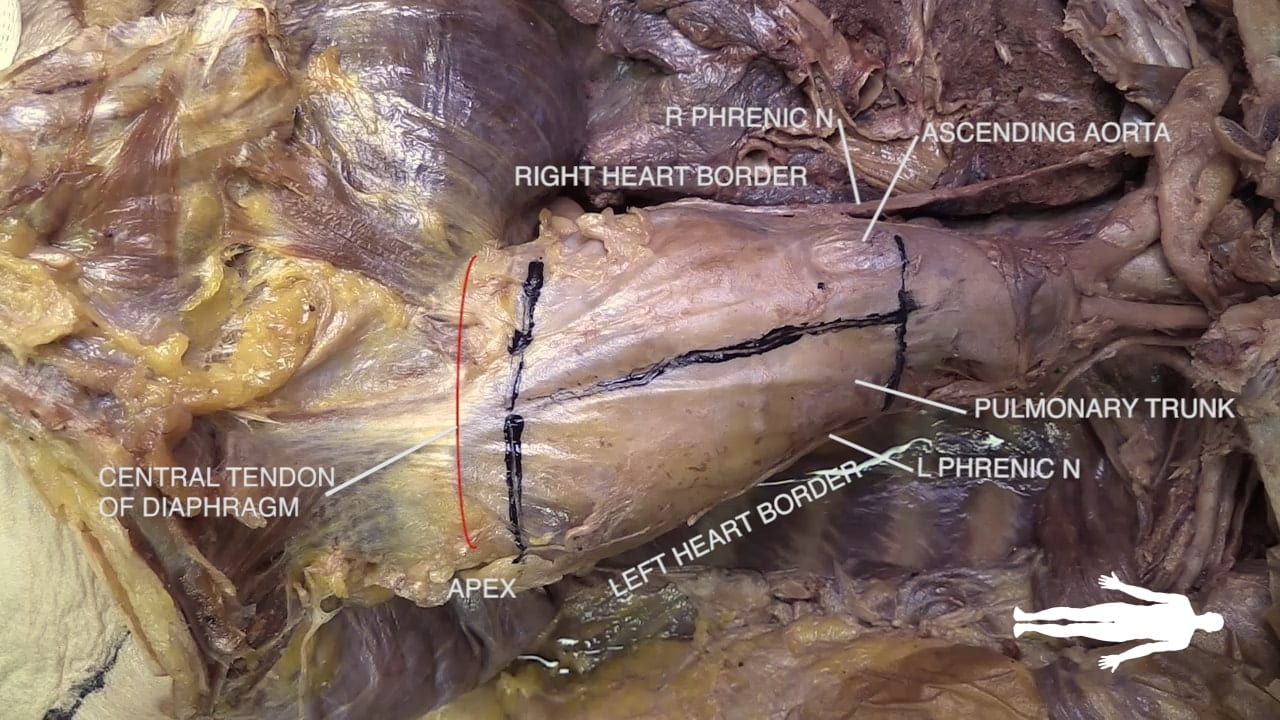
Cardiac Surfaces
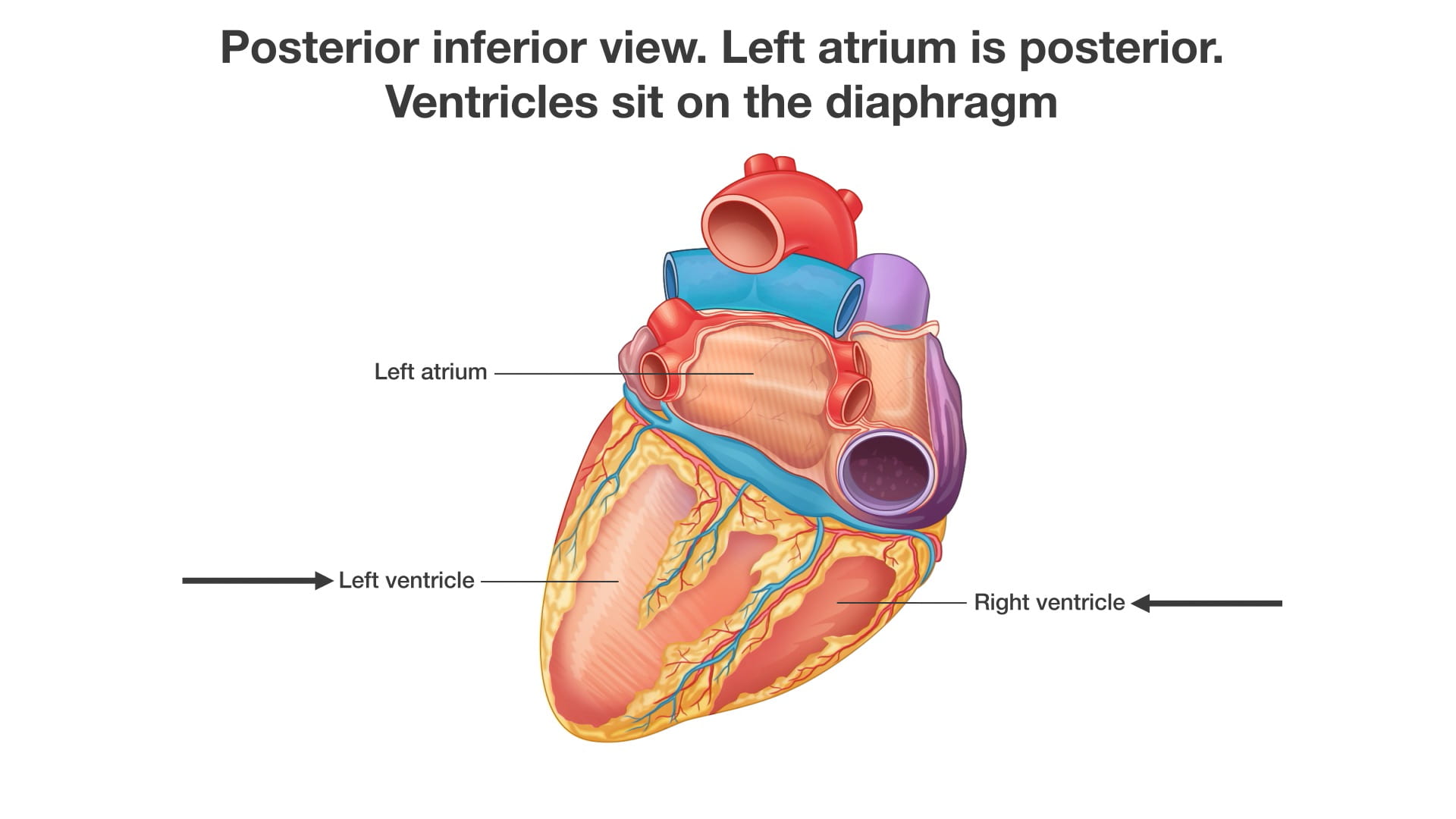
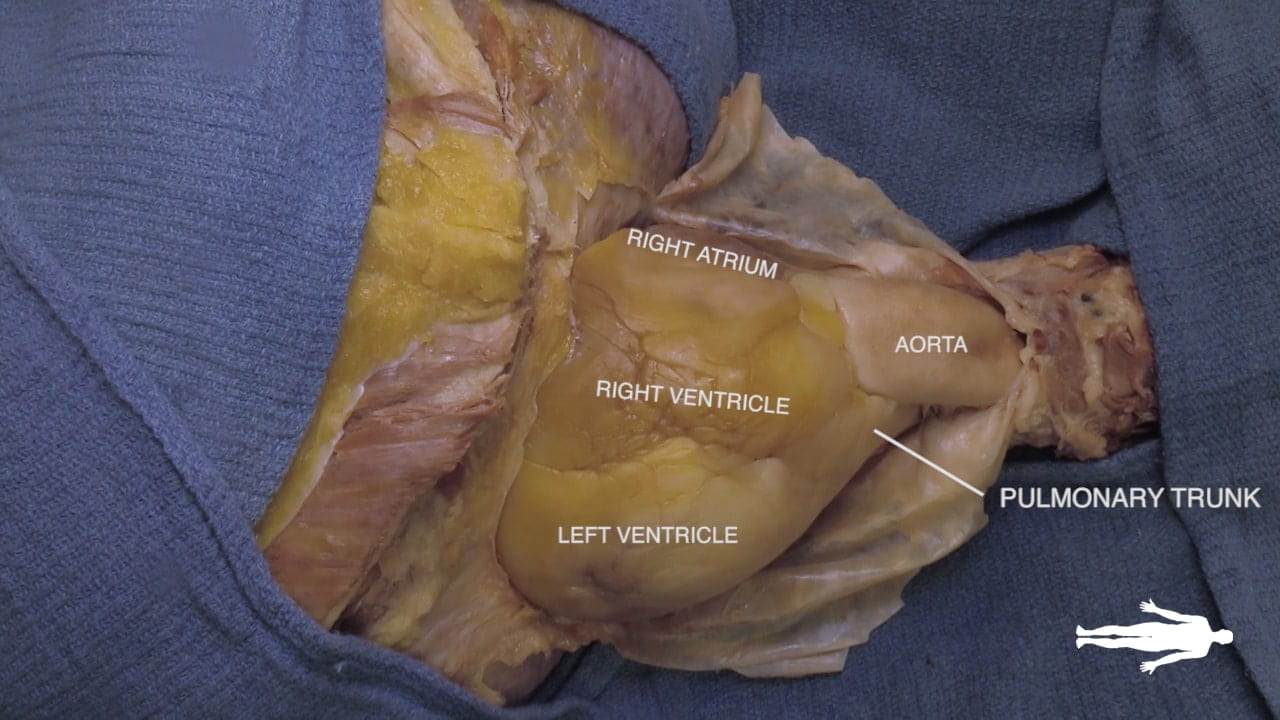
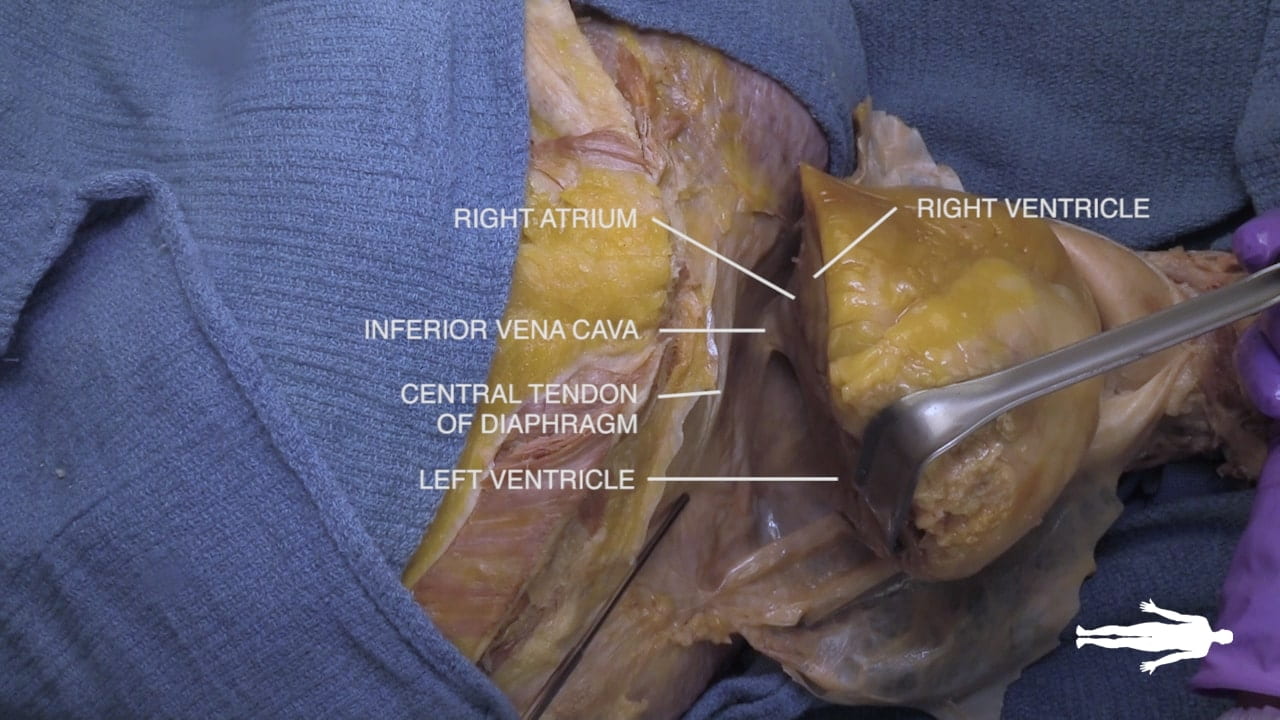
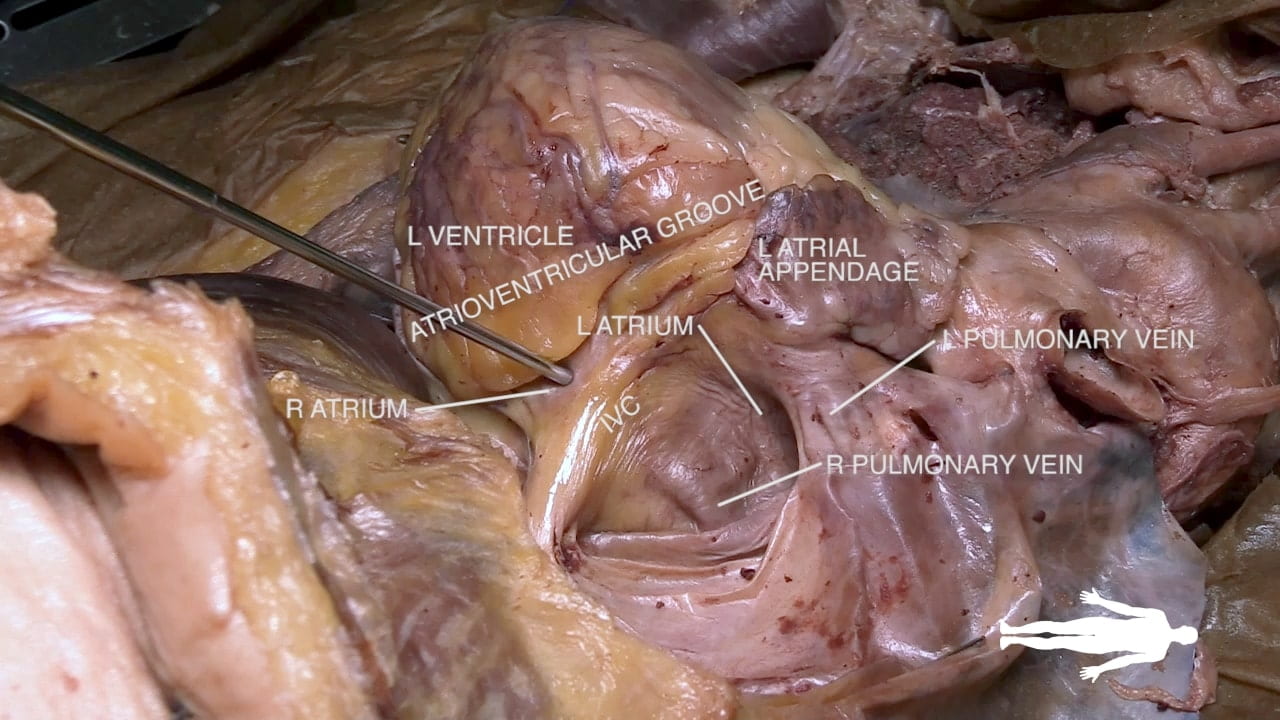
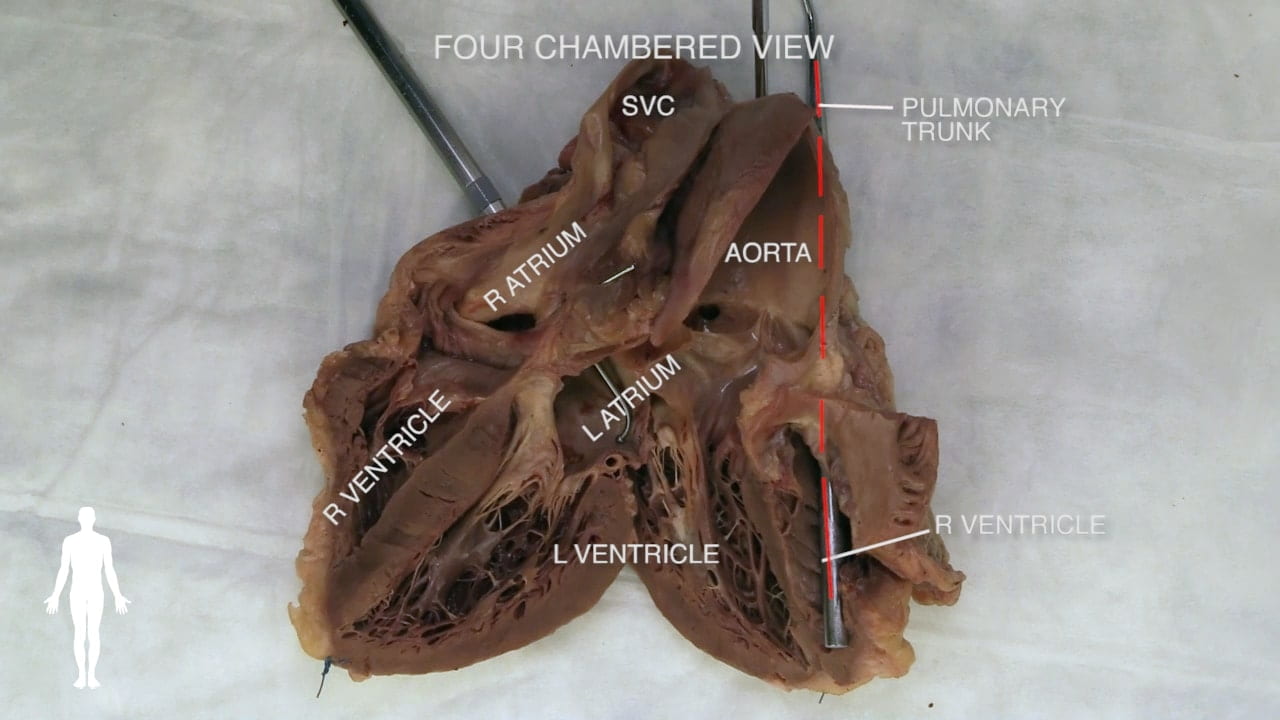
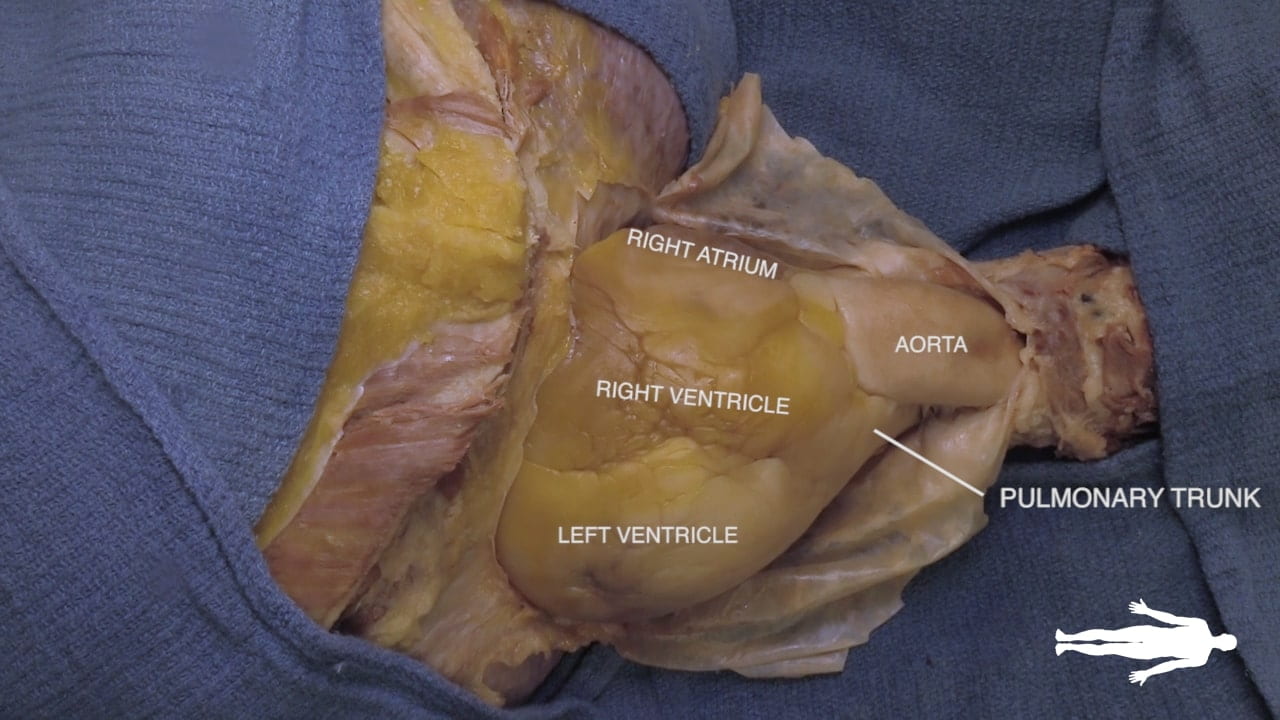
Identify the chambers of the heart, aorta, pulmonary trunk, superior and inferior vena cavae and pulmonary veins.
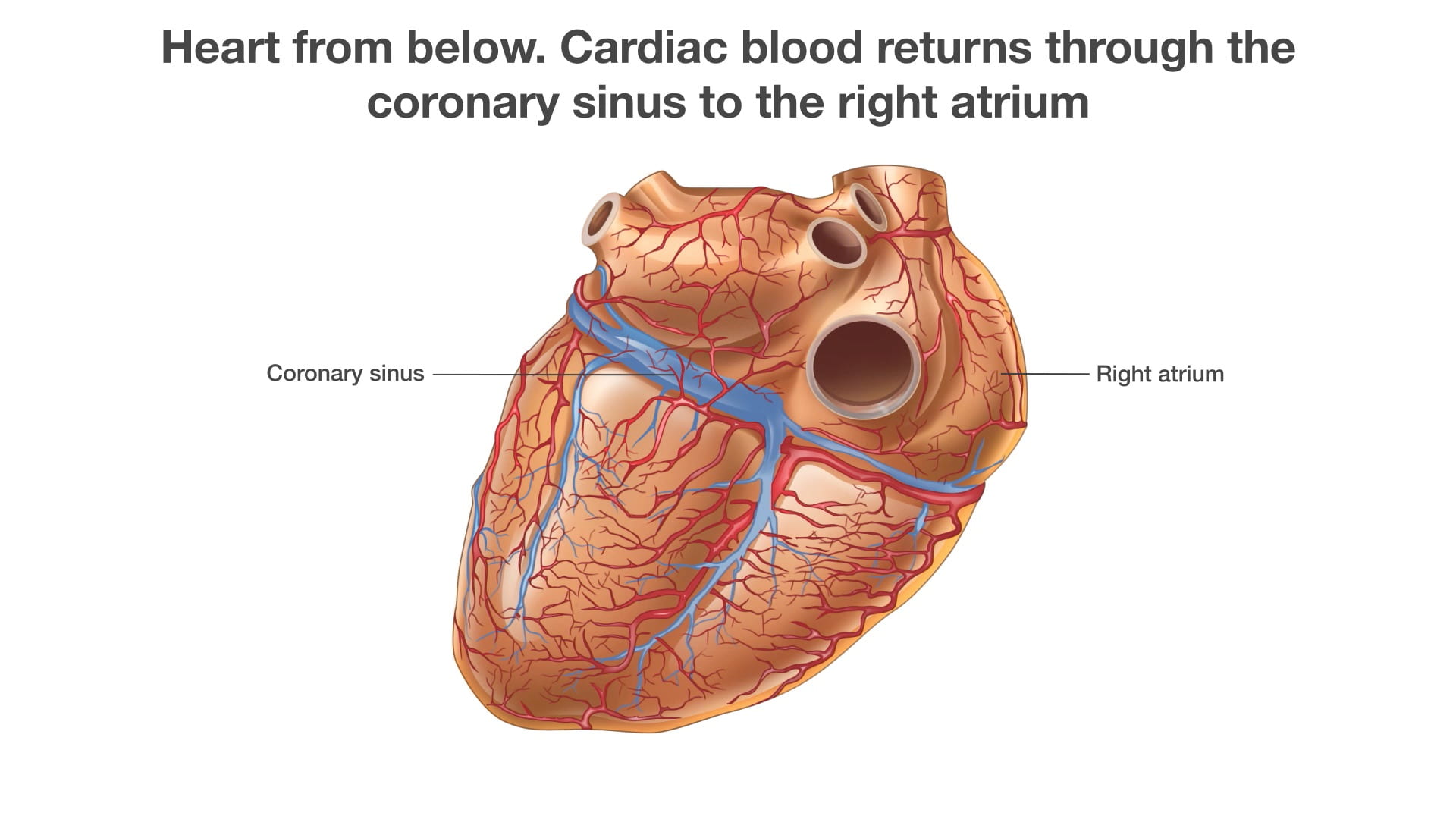
Lift the heart to view its diaphragmatic surface.
Transverse Pericardial Sinus
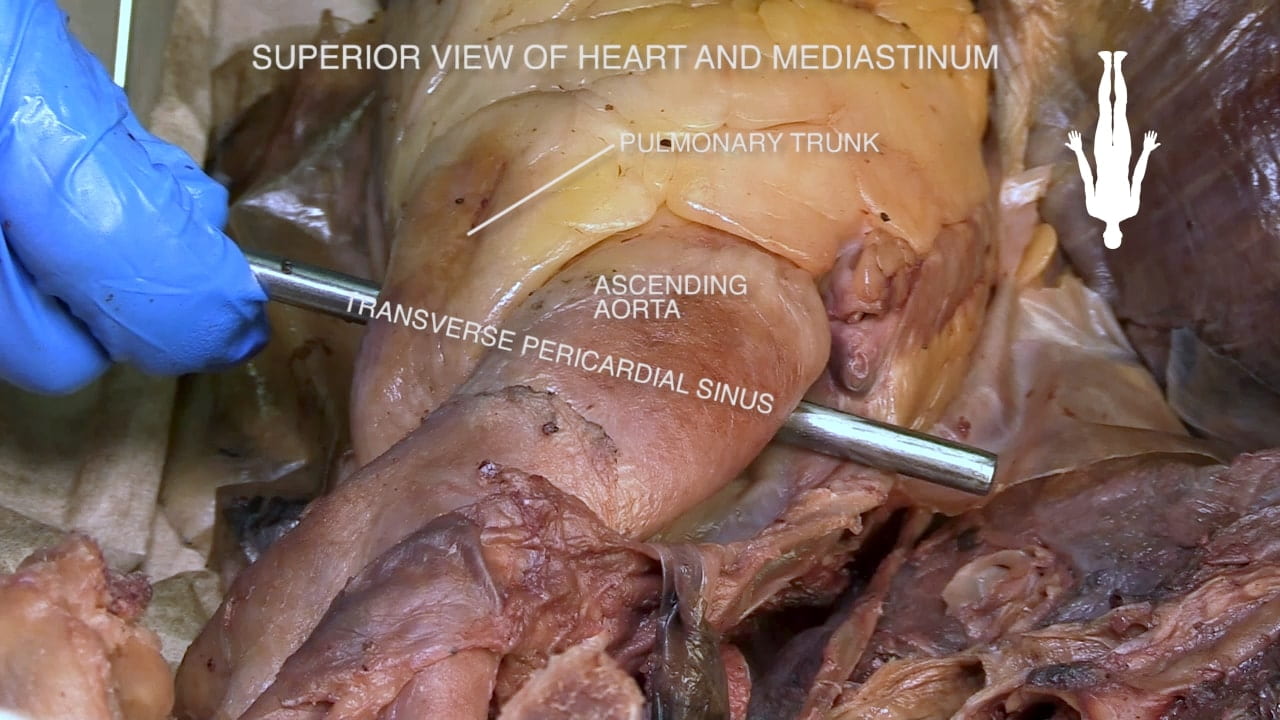
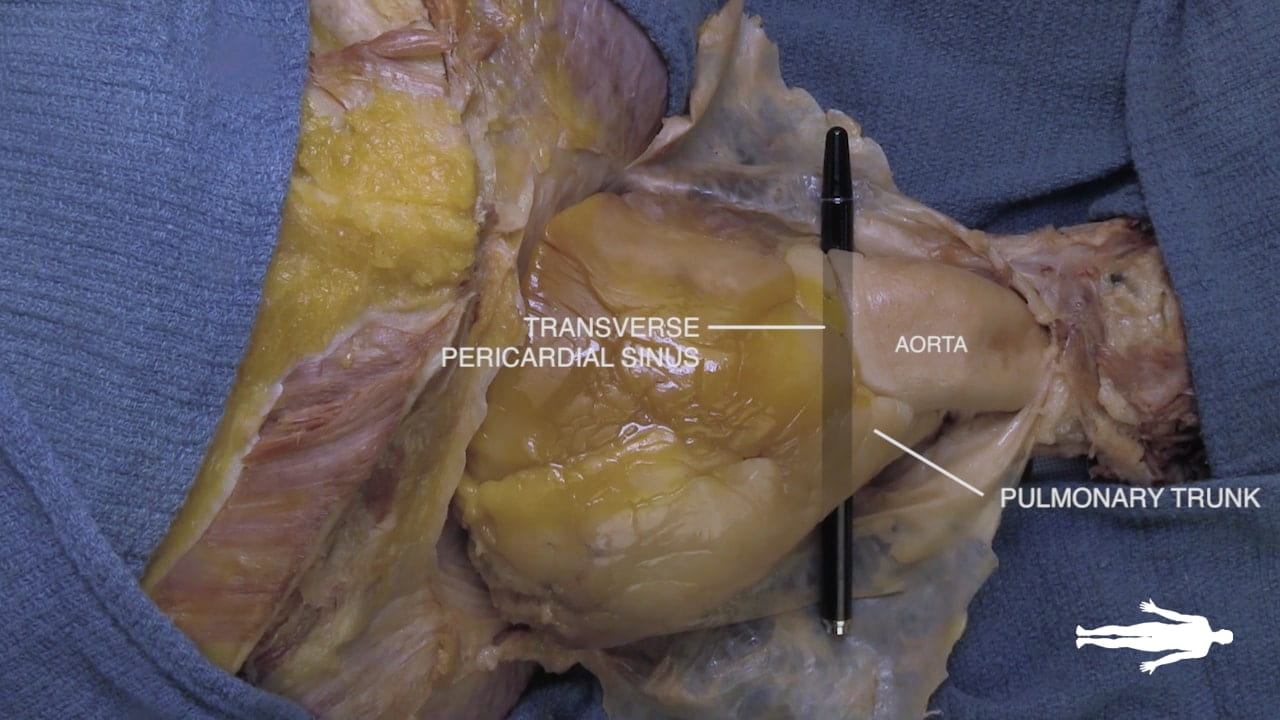
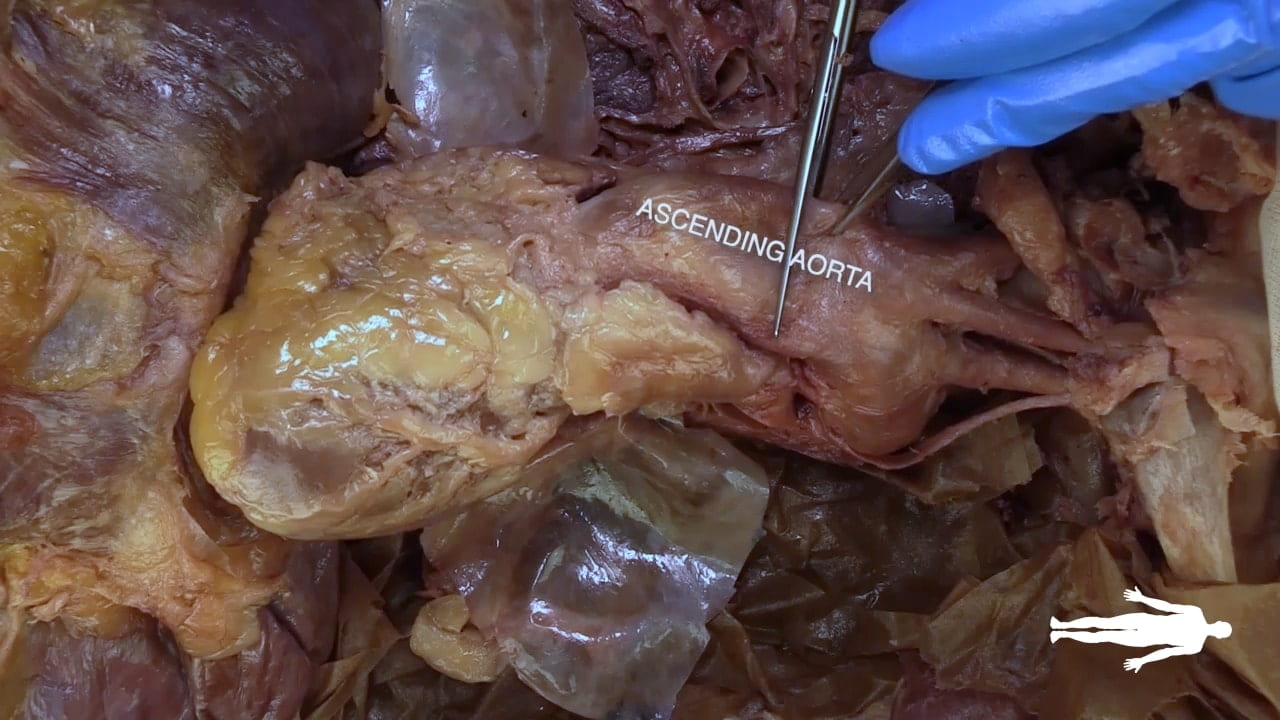
Place an instrument posterior to the pulmonary trunk and ascending aorta. Note that cardiac output is anterior to the probe and the venous inflow is posterior. This space is the transverse pericardial sinus and an important landmark in cardiac surgery.
Left Cardiac Surface
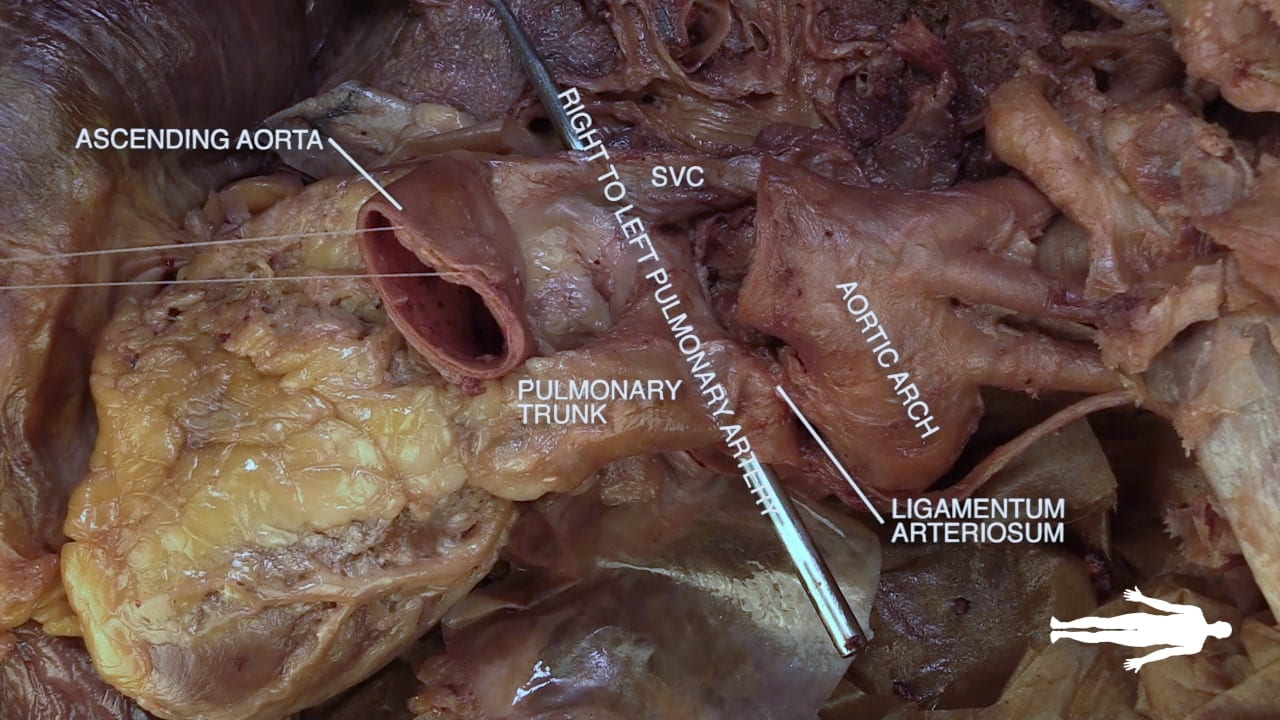
On the left side of the heart, locate vagus nerve (X), ligamentum arteriosum and left recurrent laryngeal nerve.
The vagus nerve lies along the aortic arch. The ligamentum arteriosum connects the left pulmonary artery and the arch of the aorta. The left recurrent laryngeal artery can be identified branching from the vagus nerve and passing posterior to the ligamentum arteriosum.

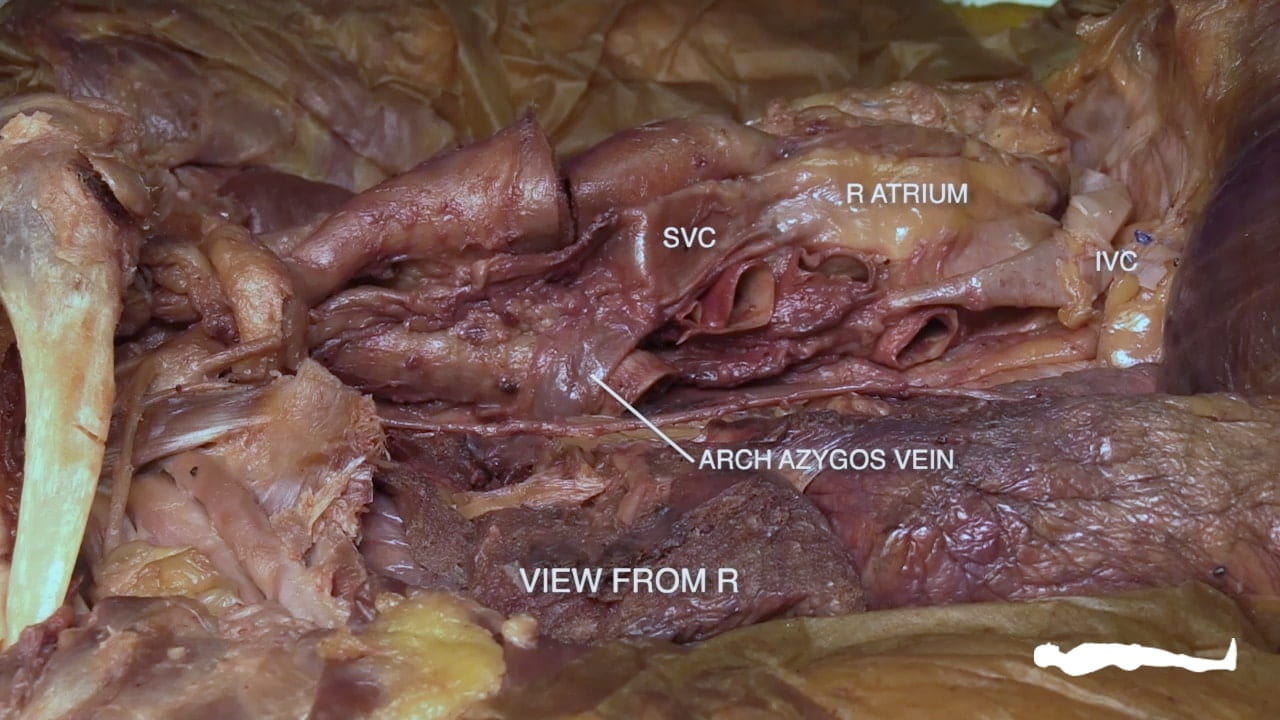
Right Cardiac Surface
On the right side of the heart, re-identify the hilus of the lung and find the arch of the azygos vein passing superior to the hilus of the lung to enter the superior vena cava.
Identify the atrioventricular groove on the right side of the heart. The right coronary artery lies in this groove.

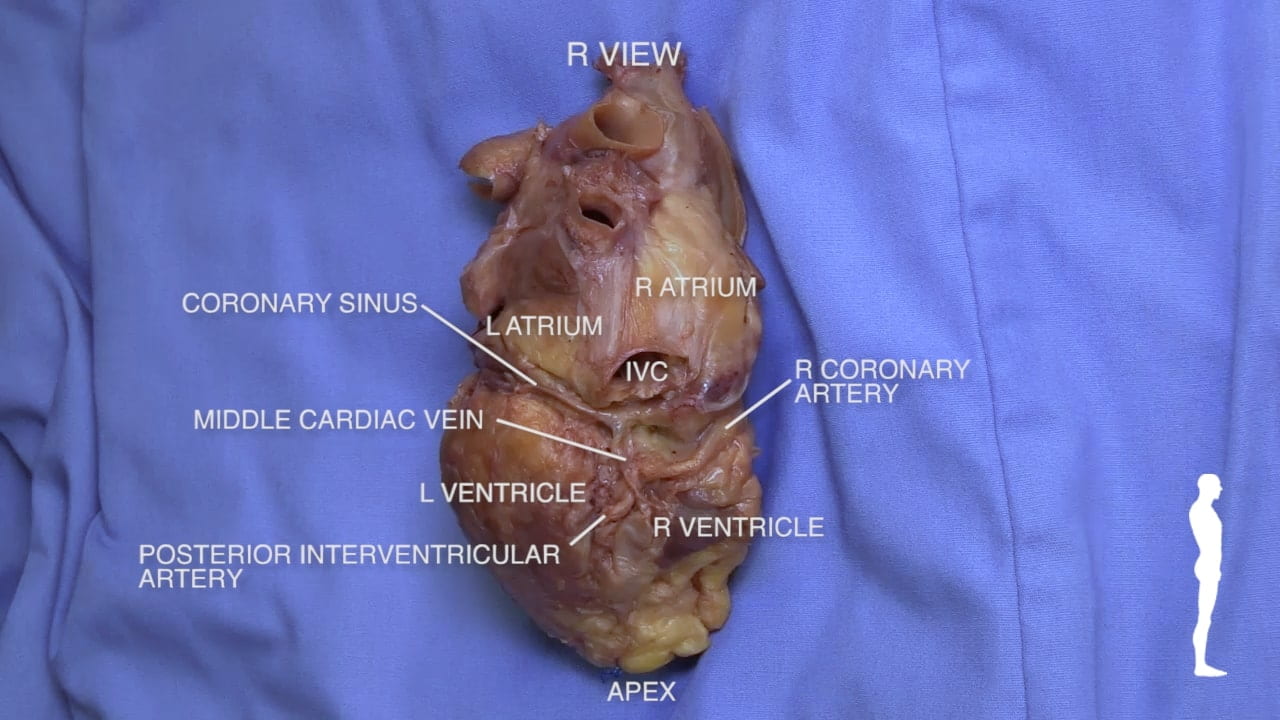
Coronary Vessels
Diagram of Coronary Vessels

Coronary Vessels
Left Coronary Artery
Removal of Heart
Removing the Heart
Bisecting the Heart
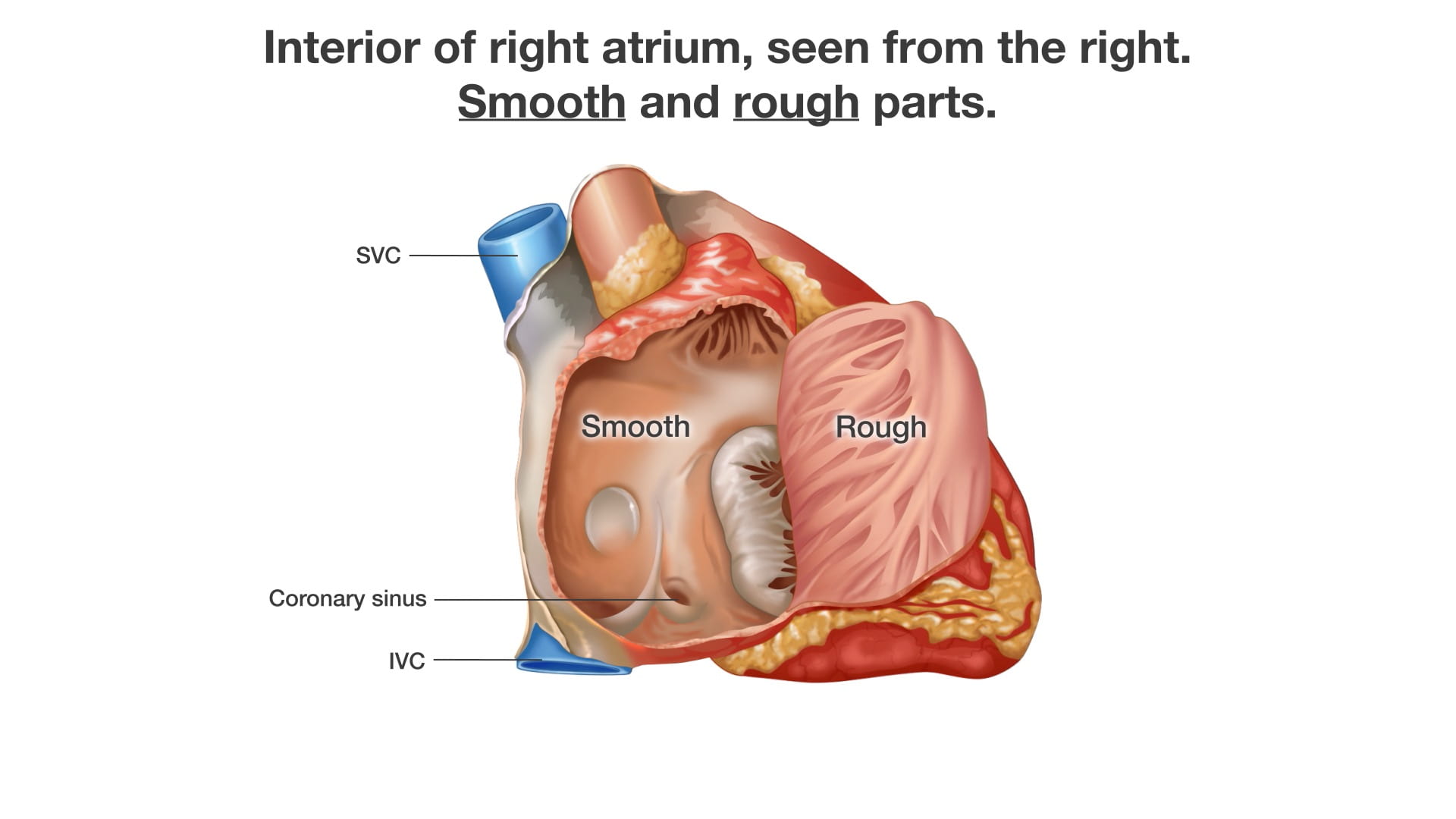
Bisecting the Heart
Cardiac Structures
In Situ Dissection
Complex in situ Dissection
Cardiac Electrical System
Physical Examination of Heart
Cardiac Clinical Correlations
Trauma: Cardiac box: The “cardiac box” is the region demarcated by the sternal notch (superiorly), xiphoid process (inferior), and midclavicular lines (laterally). Penetrating trauma or blunt force to the cardiac box can injure the heart. The right ventricle, being the most anterior structure of the heart, is most prone to penetrating injury. A life-threatening consequence of cardiac trauma is cardiac tamponade where blood accumulates within the pericardial sac and compresses the heart. For more information of thoracic trauma, review the “deadly dozen”.
Procedure: Atrial fibrillation, the left atrial appendage, and TEE: Atrial fibrillation (Afib) impairs the contraction and emptying of the atria which allows blood to pool and clot. These clots generally form in the left atrial appendage (LAA), a pouch-like portion of the left atrium. Return to sinus rhythm can dislodge clots into the aorta (causing stroke) therefore high-risk patients should undergo work-up for LAA thrombus prior to cardioversion. Because its far posterior location and interference from the bones of the spine/rib cage, the left atrium cannot be reliably viewed through transthoracic echo (external ultrasound probe placed on external chest). Importantly, the esophagus is located immediately posterior to the left atrium, Therefore, the gold-standard for diagnosing LAA thrombus is transesophageal echo (TEE) which entails passage of an ultrasound probe through the mouth and into the esophagus of an anesthetized patient.
Embryology: Foramen ovale and ductus arteriosus: In utero, lungs are fluid-filled (i.e. high-pressure system) therefore most blood pumped by the right heart bypasses the lungs through two structures:
- the ductus arteriosus: allows blood to move from pulmonary artery to aorta
- the foramen ovale: allows blood to move from the right atrium to the left atrium
At birth, the lungs become a low-pressure system prompting signaling events that precipitate closure of these structures to leave remnants:
- ductus arteriosus becomes the ligamentum arteriosum
- fossa ovalis becomes the foramen ovale
If these structures remain inappropriately open (i.e. patent), inappropriate shunting of blood may occur. A patent ductus arteriosus (PDA) allows blood to move from the higher-pressure aorta to the lower pressure pulmonary trunk, pathologically increasing blood flow across the heart and lungs. A patent foramen ovale (PFO), while usually asymptomatic, is associated with intermittent right to left shunting when RA pressure rises (see paradoxical emboli for more information).
Surgery/Autopsy: Cardiac surgery and phrenic nerve: Within the thorax, the right and left phrenic nerves pass between the fibrous pericardium and the mediastinal parietal pleura. As a result, cardiac surgeries that involve manipulation of the pericardium carry a risk of phrenic nerve injury. Clinical presentations include hiccups and difficulty breathing. Imaging may show diaphragmatic dysfunction, paralysis, or paradoxical movements.
Anatomical Variations: Coronary “dominance”: The posterior descending artery (PDA) feeds the posterior third of the interventricular septum. The PDA arise from the right coronary artery (70%; “right-dominance”), left coronary artery (10%; “left-dominance”), or both (20%; “co-dominance”). Knowing a patient’s cardiac dominance is critical for appropriate endovascular navigation to alleviate PDA stenosis or appropriate installation of vascular grafts during bypass surgery.
Imaging: Chest Xray is the first modality often used to image the chest, as it is fast, safe and inexpensive. However, although good for looking at large lung findings and assessing the size of the heart or placement of support devices, it does not allow for visualization of discrete cardiac anatomy. Instead, CT with contrast can be use. Echocardiogram (ultrasound) is one of the best and most common ways to evaluate the cardiac chambers and function. Cardiac MRI can be used for specialized applications to evaluate the myometrium and cardiac function, but requires much more time and is only performed at subspecialty centers.
Imaging correlate: Head to Table 13 to see a pacemaker or Table 26 to see a pacemaker, cardiac valve replacement (can you figure out which one?) and other support devices. What anatomic structures are these support devices located in? Challenge: How are the cardiac pacemaker leads placed via an endovascular approach…how did they get there??
Images (Click to Enlarge)


Autopsy images showing knife wound to heart (L) and laceration from fractured ribs (R)

TEE showing thrombus (arrow) in LAA

Autopsy image showing PFO; probe passing from RA side to LA side through opening

Fetal cardiac physiology

Autopsy image showing acceleration-deceleration aortic laceration; notice site of tear is the aortic isthmus (just distal to subclavian take-oT)

Autopsy images showing cardiac tamponade