Retroperitoneum
Lab Summary
The retroperitoneum along with its organs, glands, vasculature and nerves are taught. The retroperitoneal structures of the right and then left are presented sequentially emphasizing anatomic organization, differences between sides and circulation.
Lab Objectives
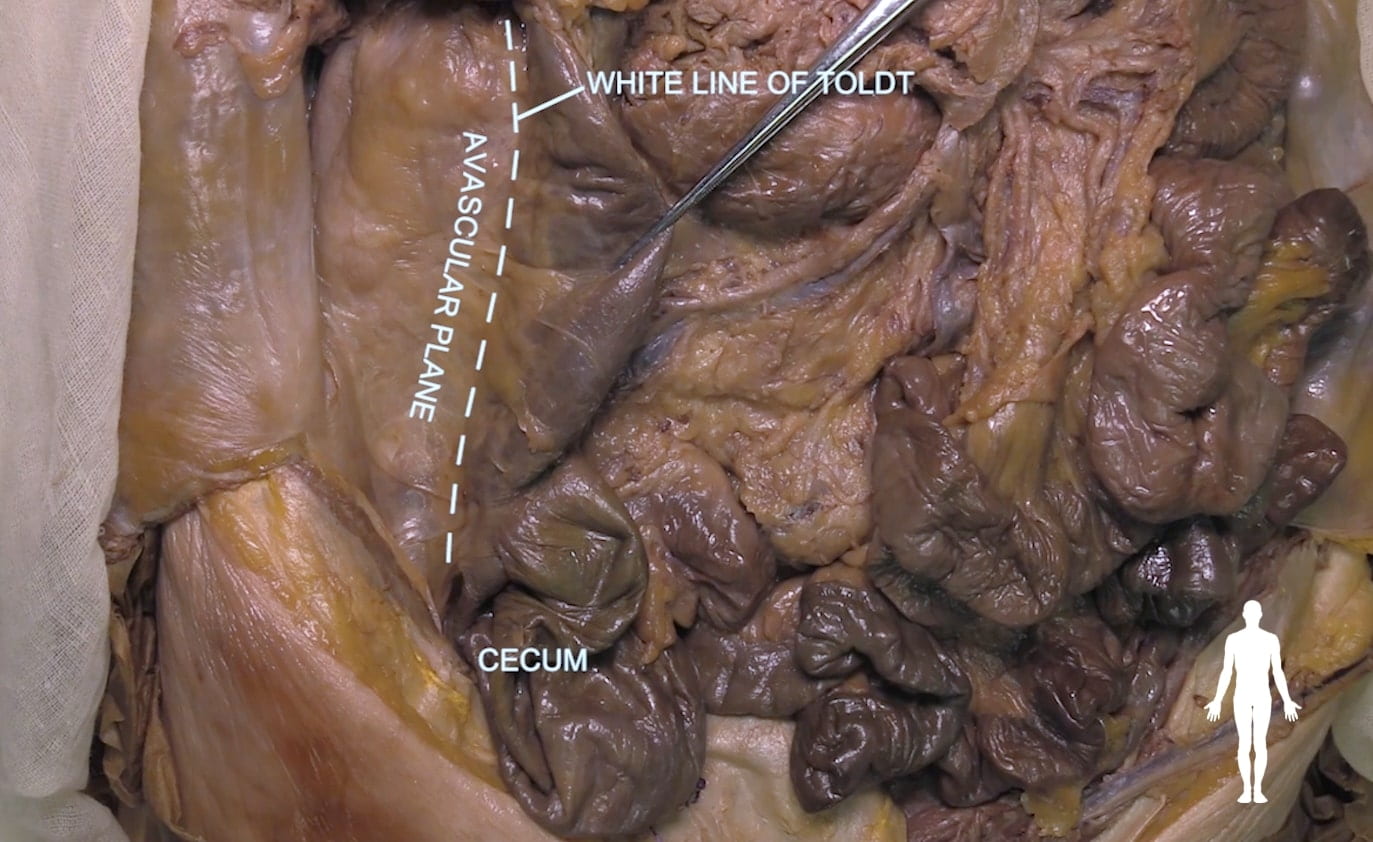
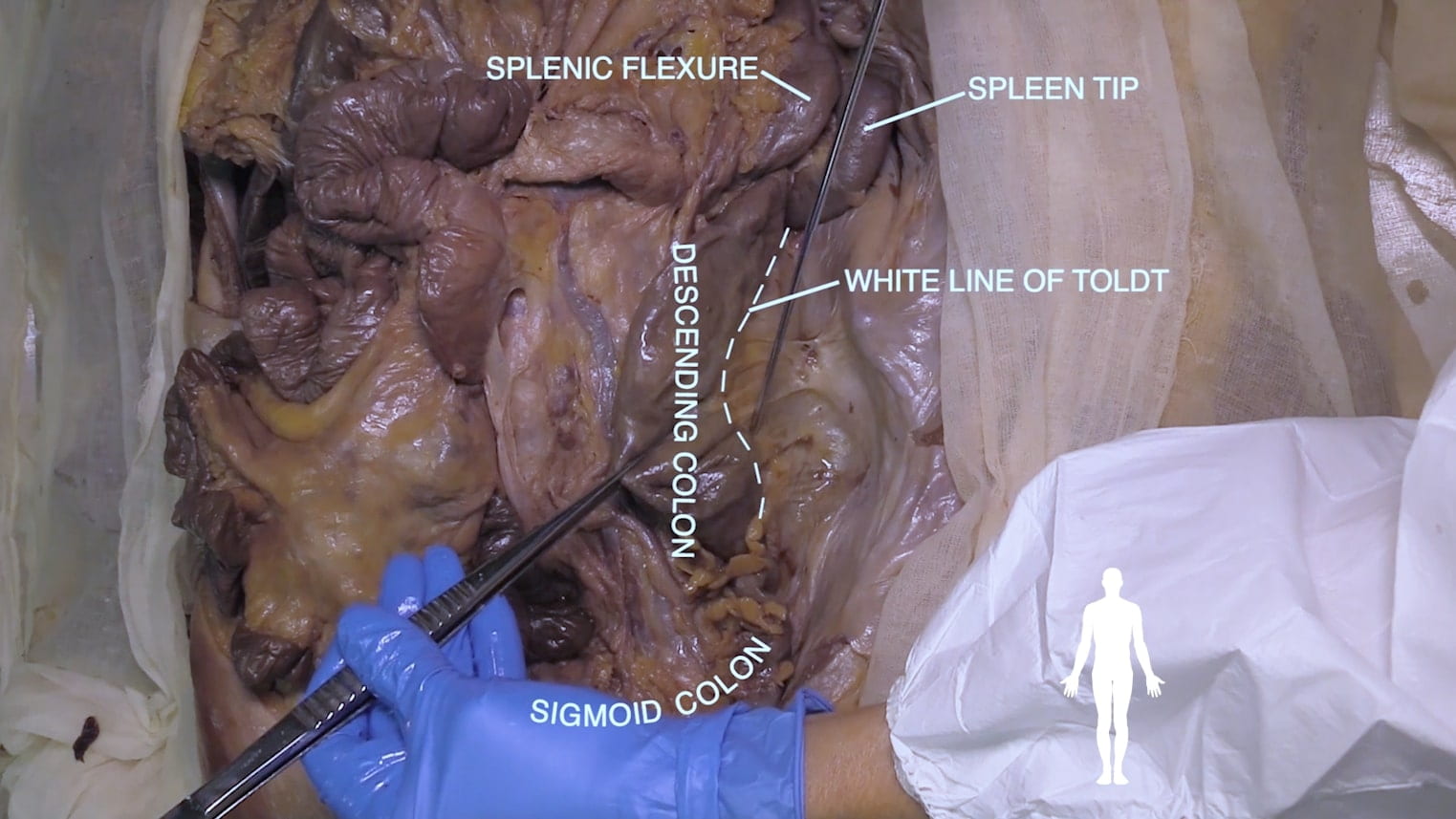
- Understand the significance of the white line of Toldt.
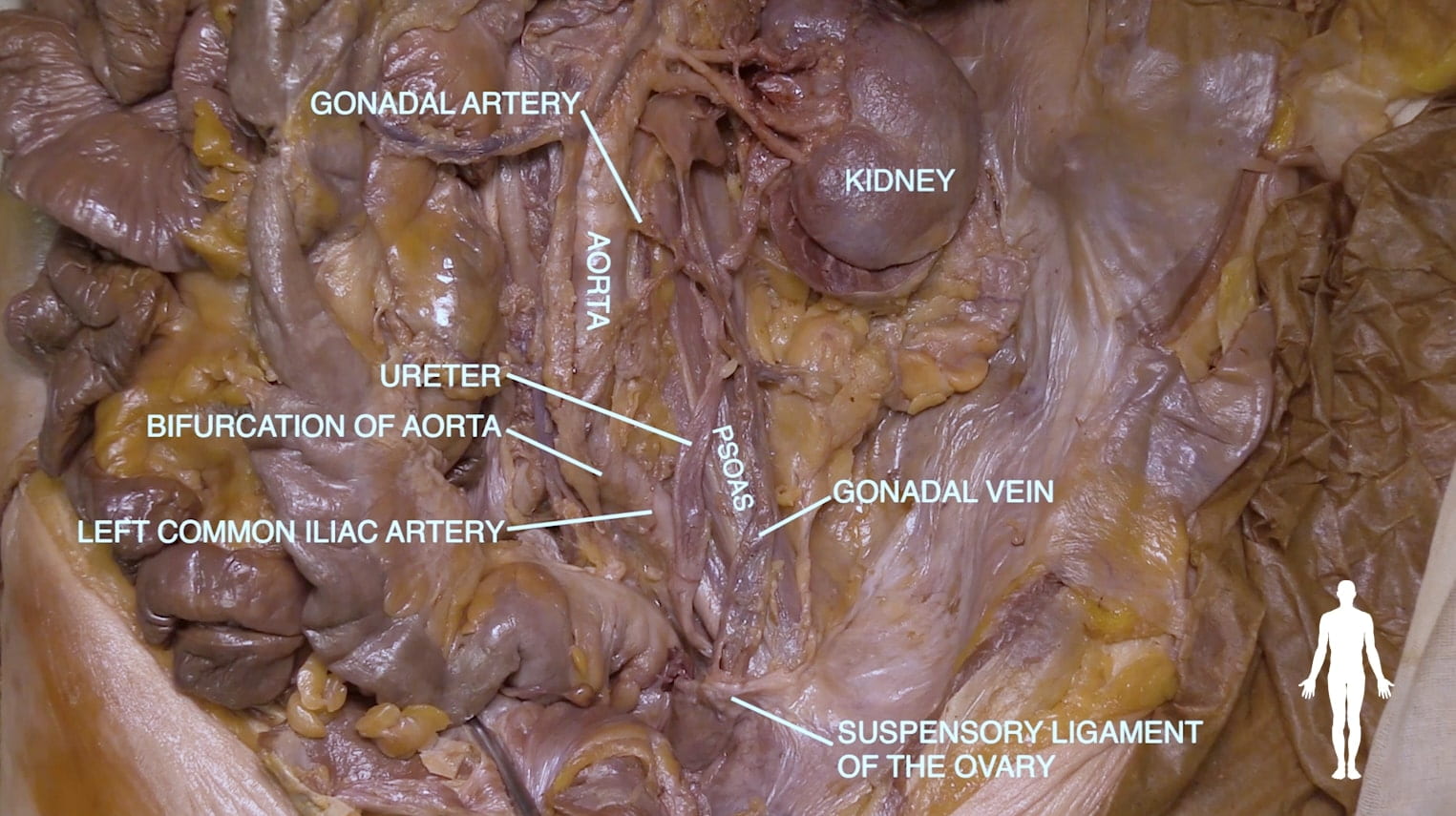
- Describe the course of the ureter.
- Describe the auscultation site for the renal arteries.
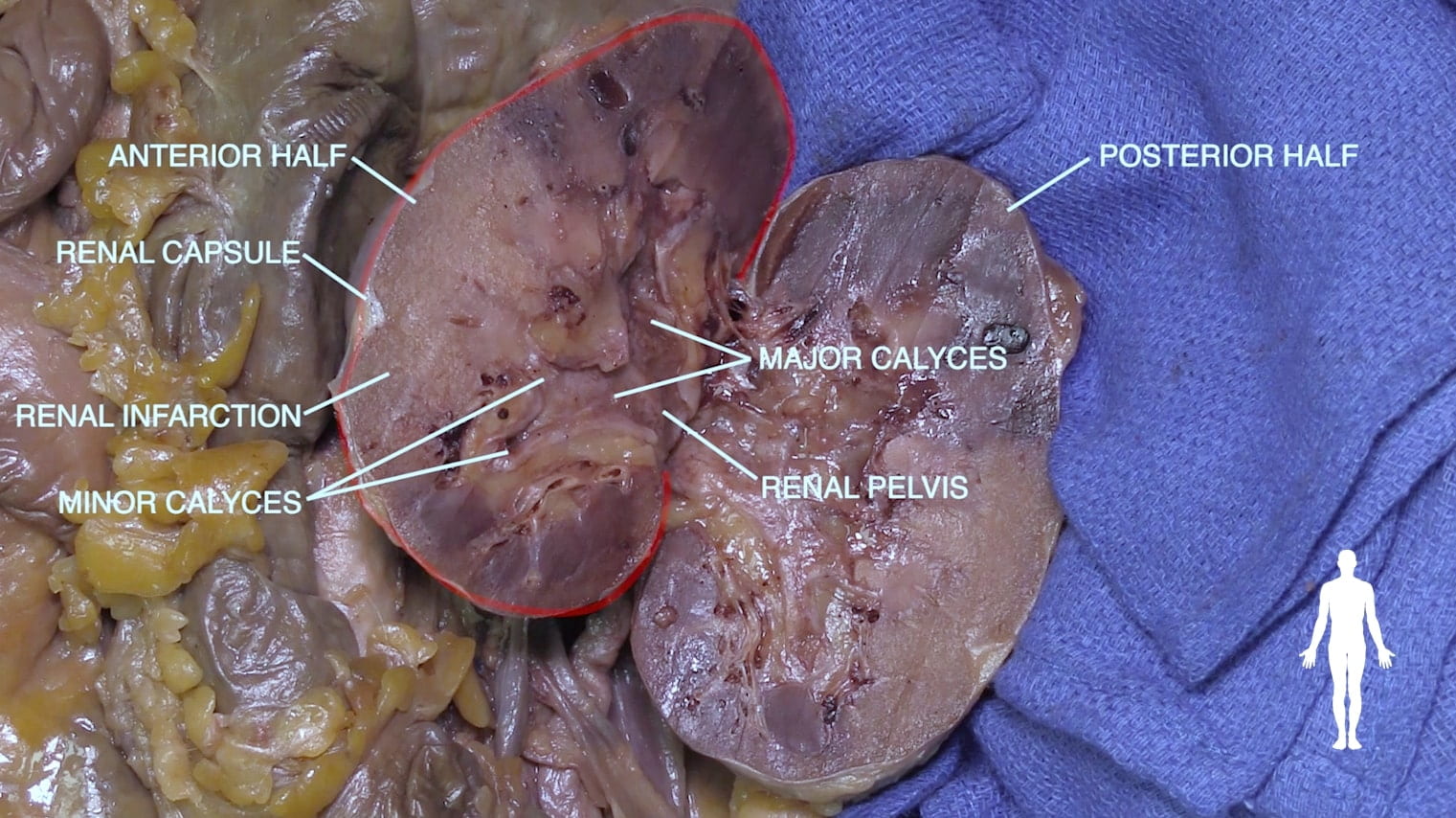
- Describe the macroscopic internal structure of the kidney.
- Describe the position of the adrenal gland.
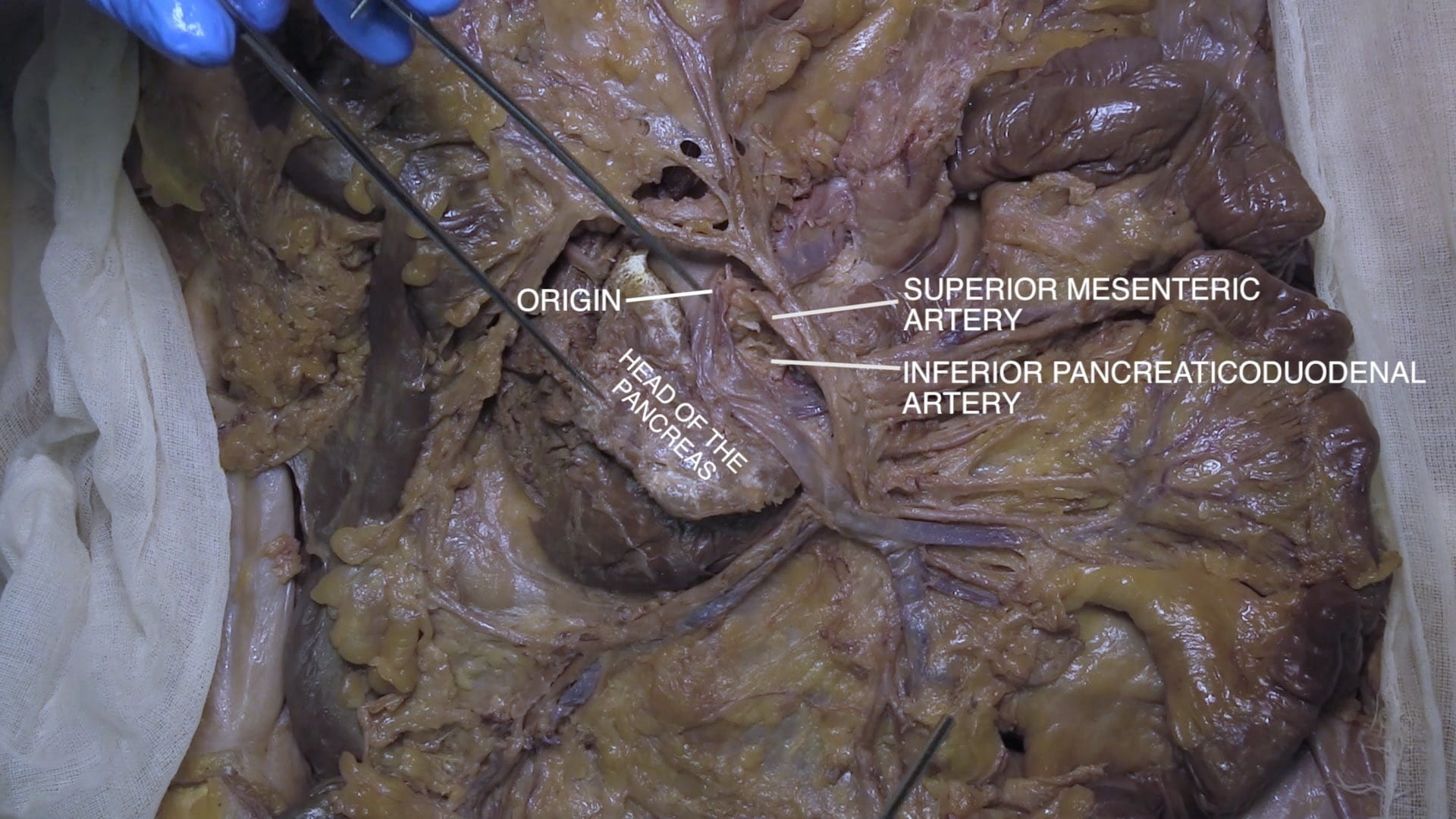
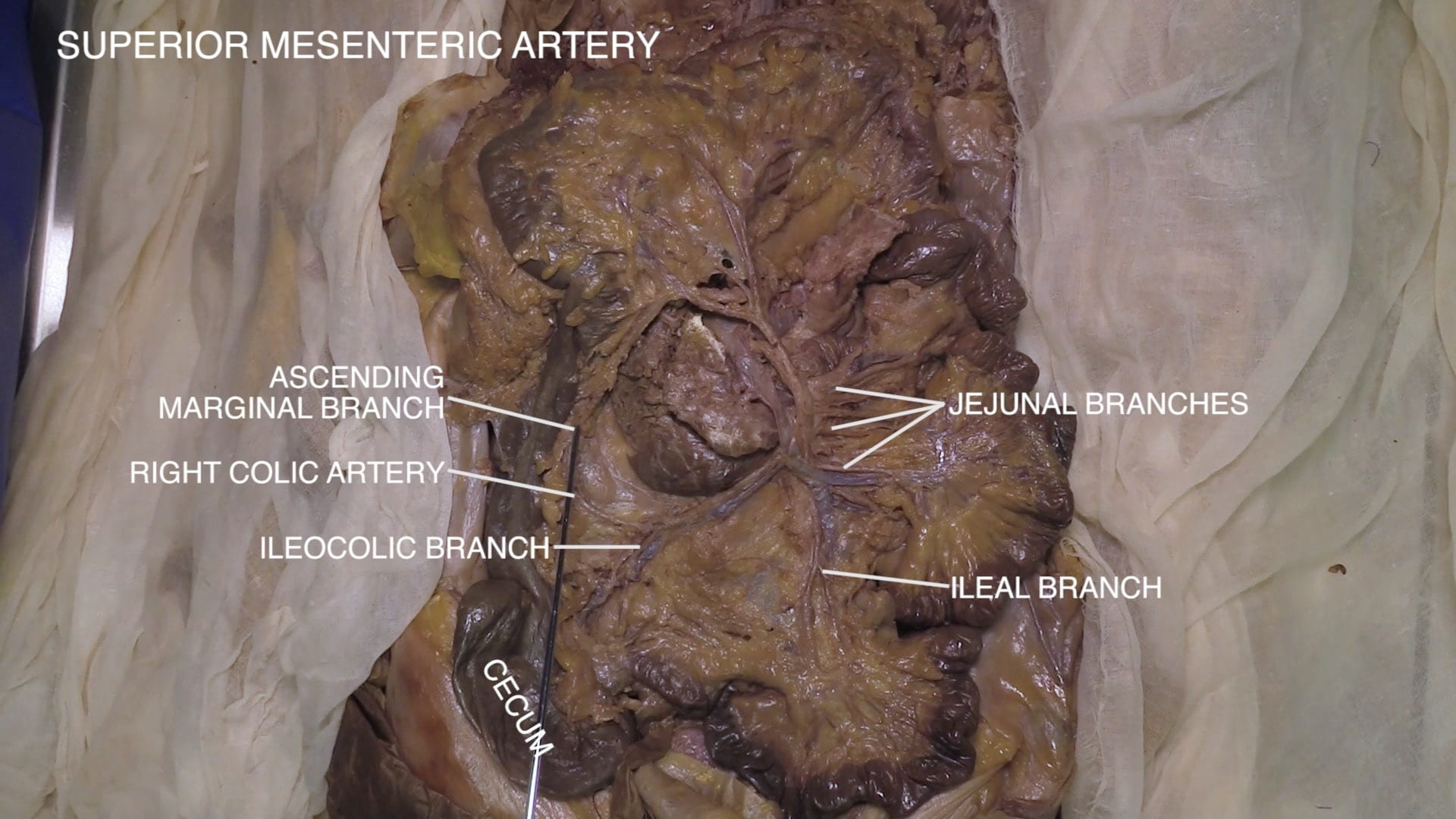
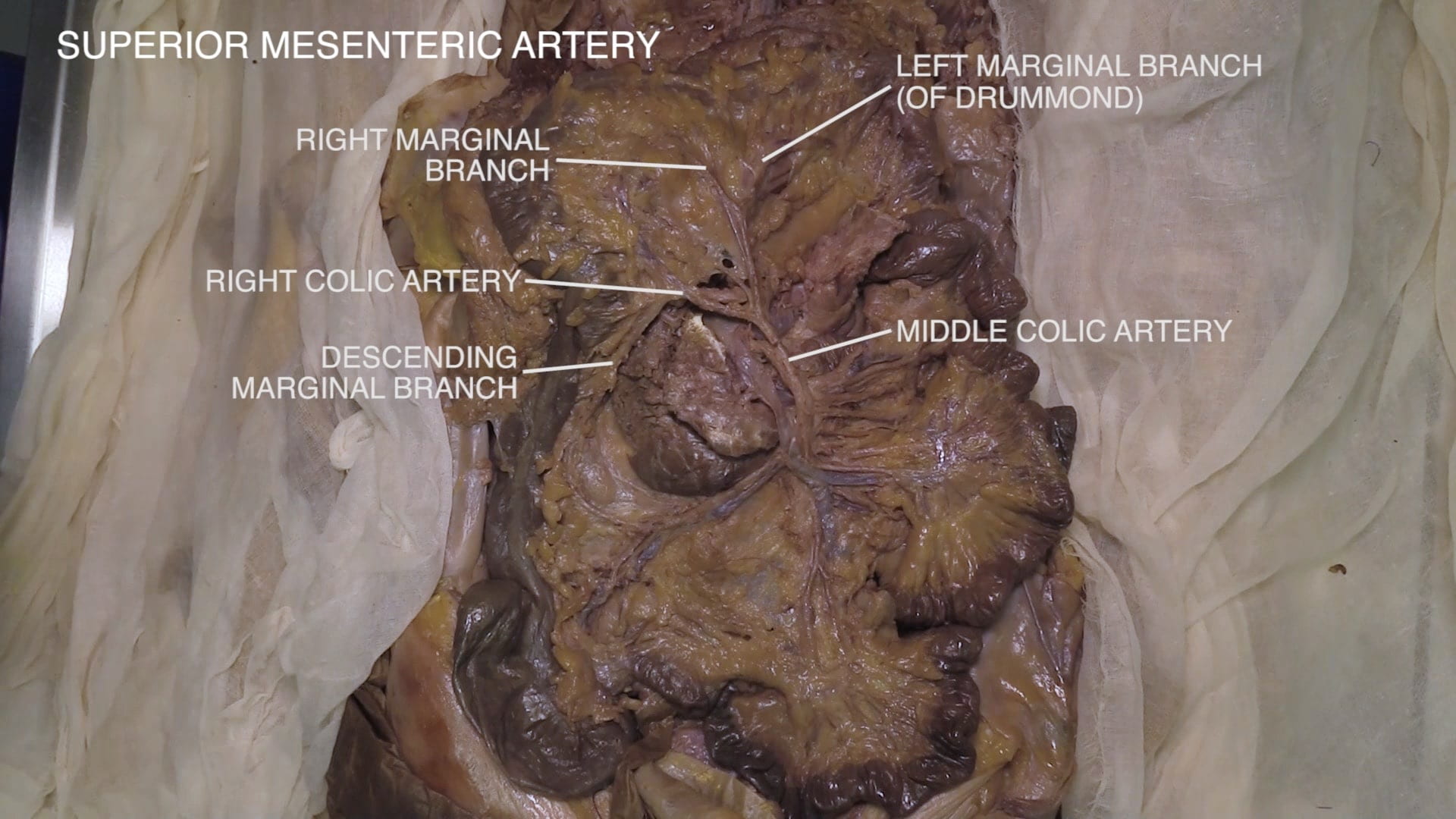
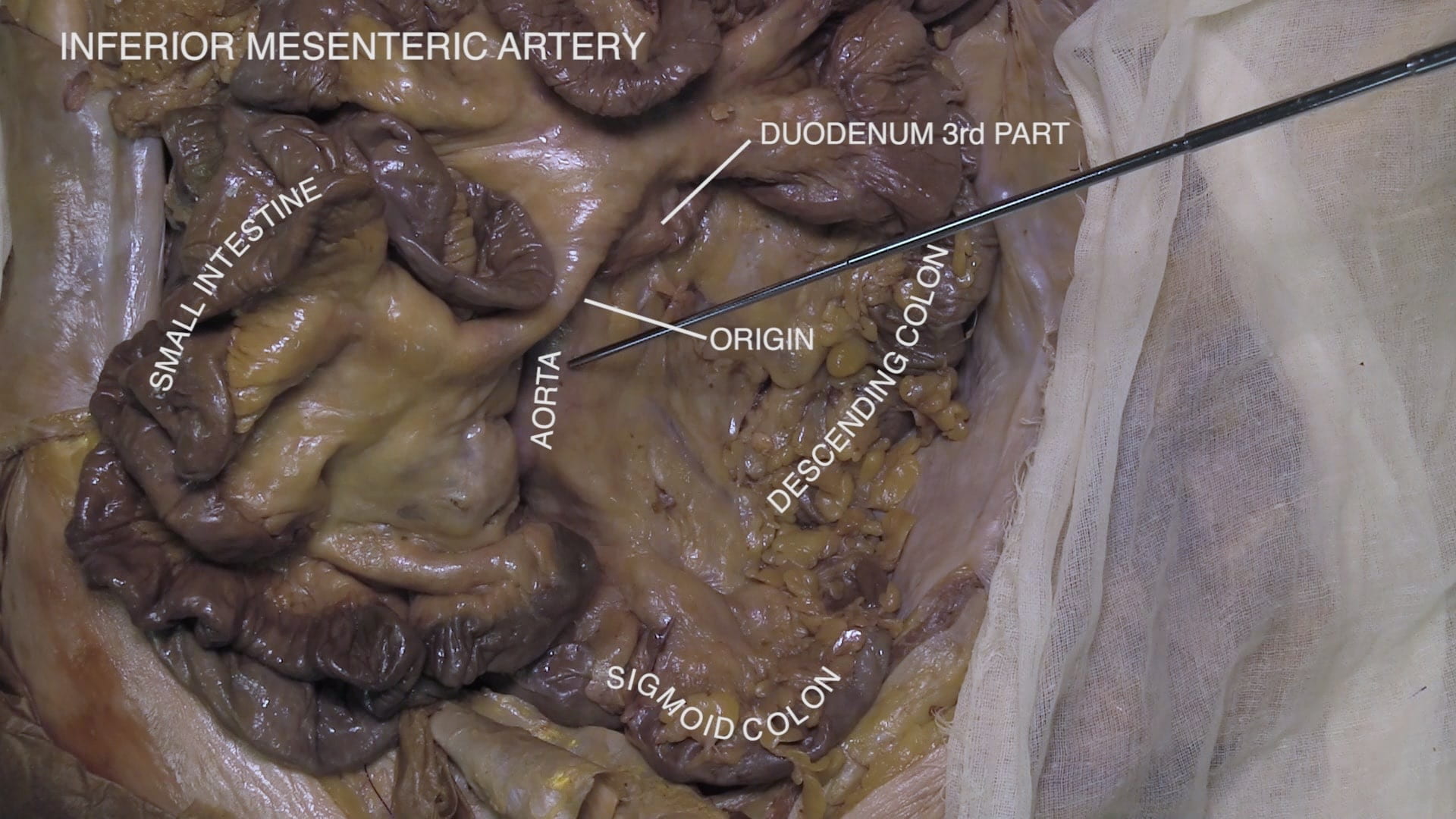
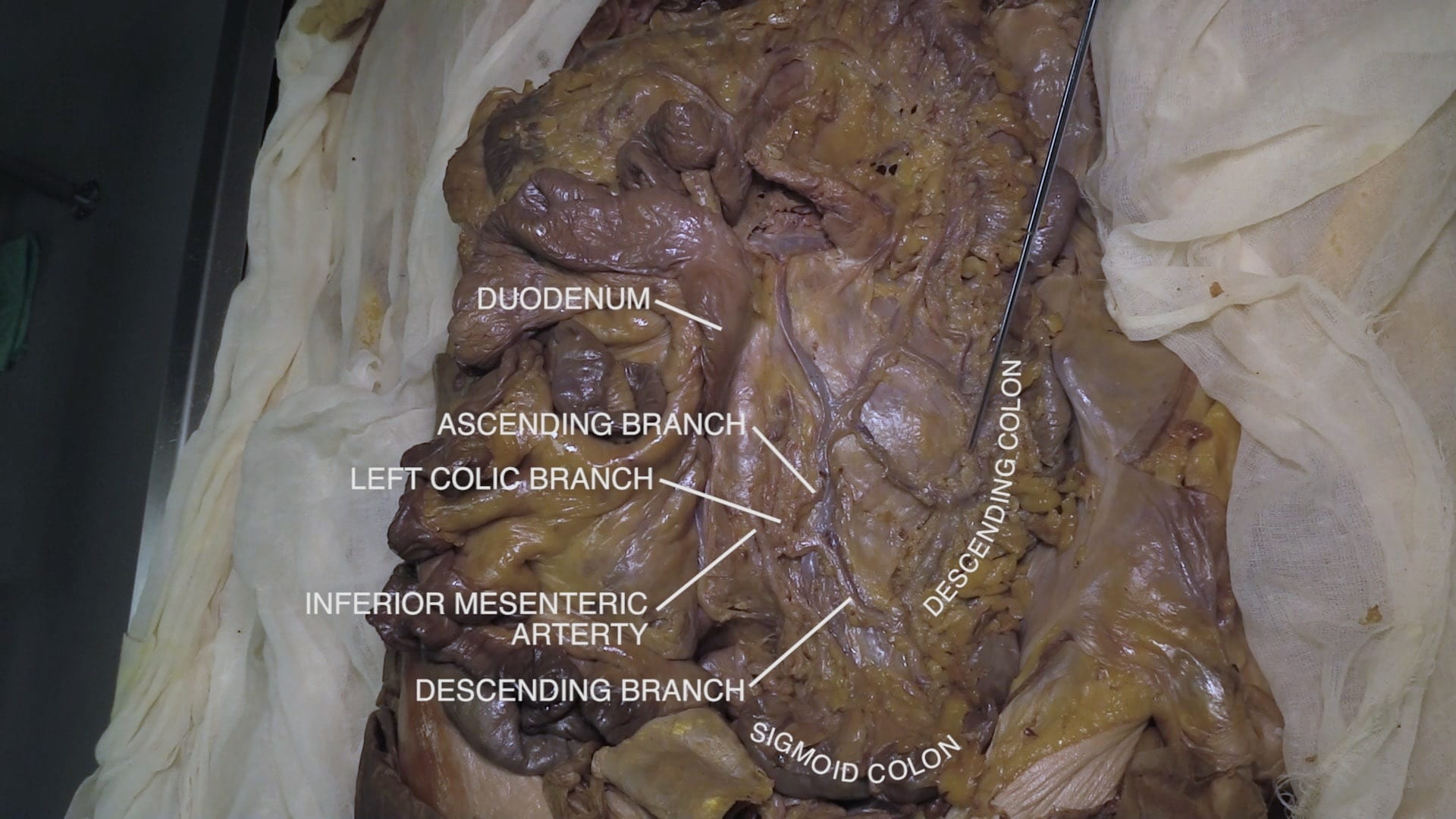
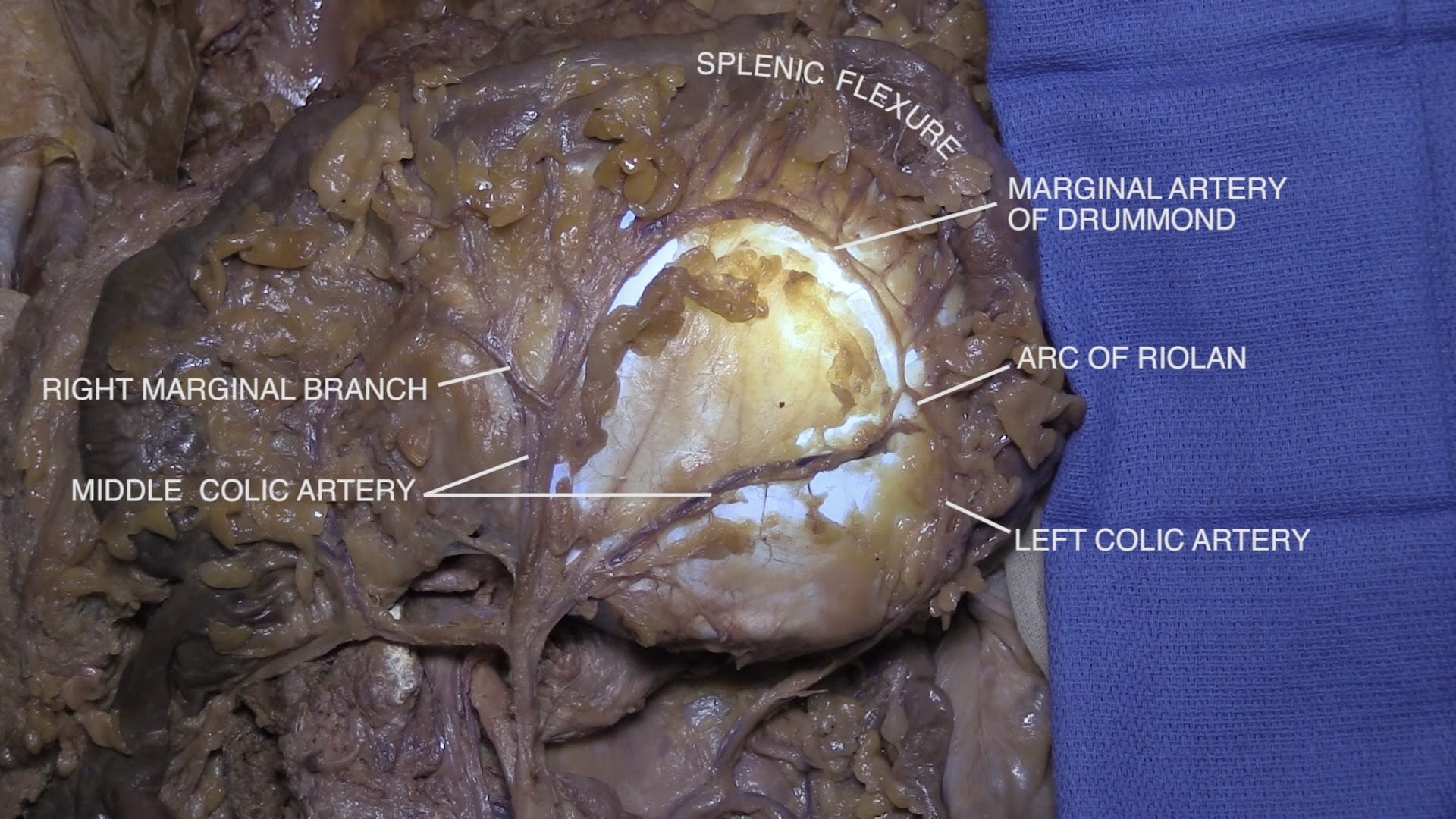
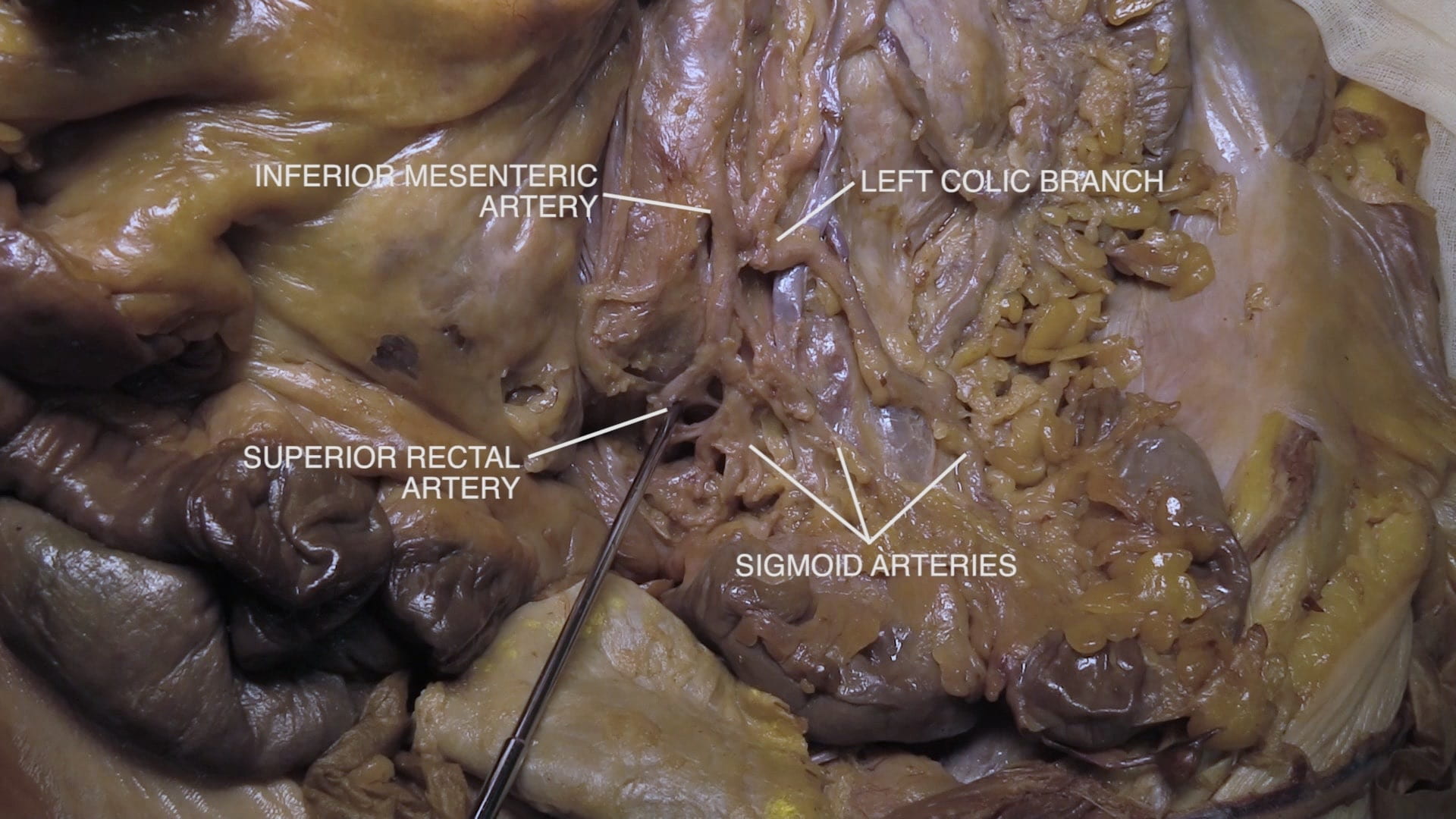
- Be able to describe the distribution of the celiac, superior mesenteric and inferior mesenteric arteries.
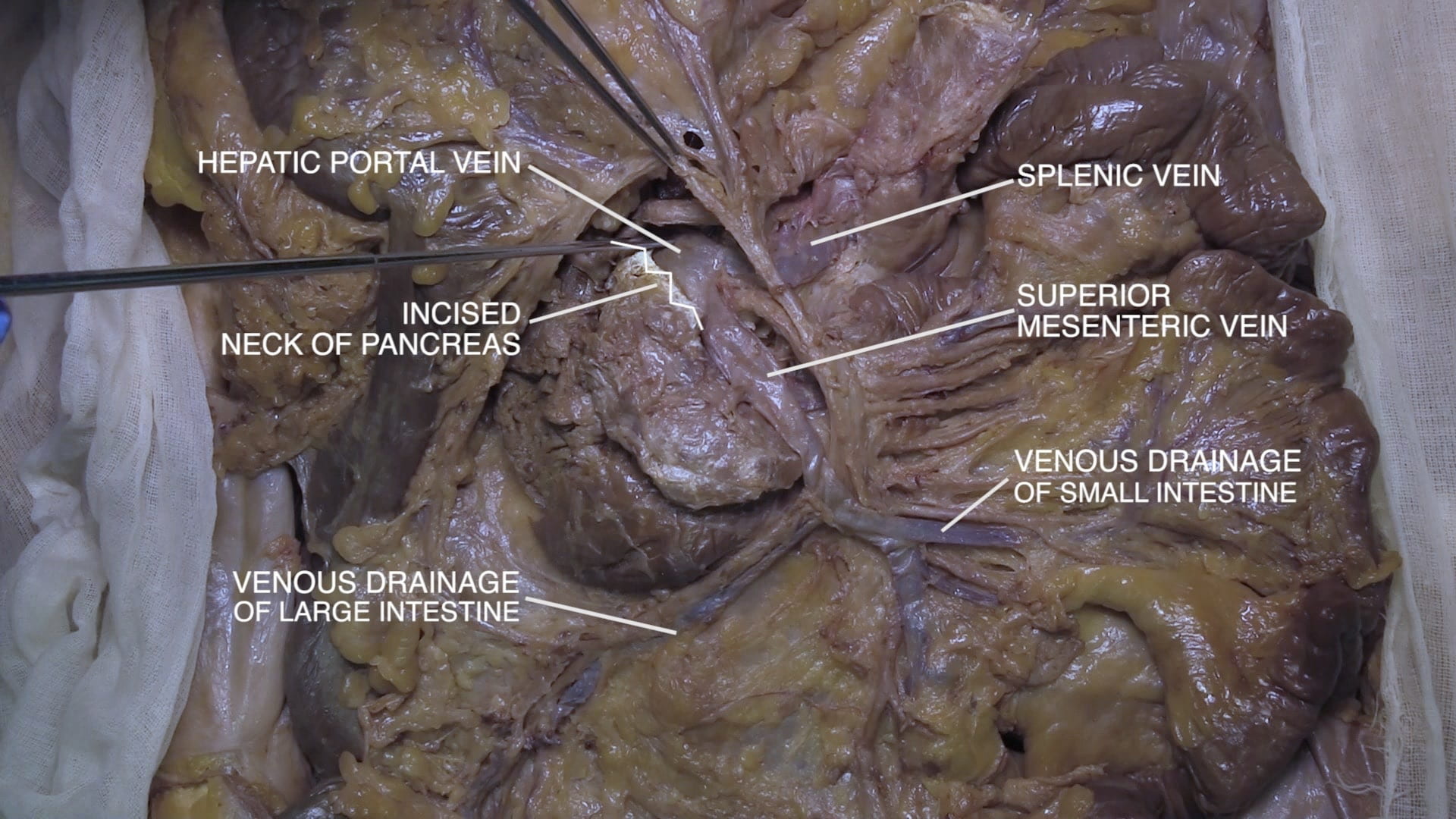
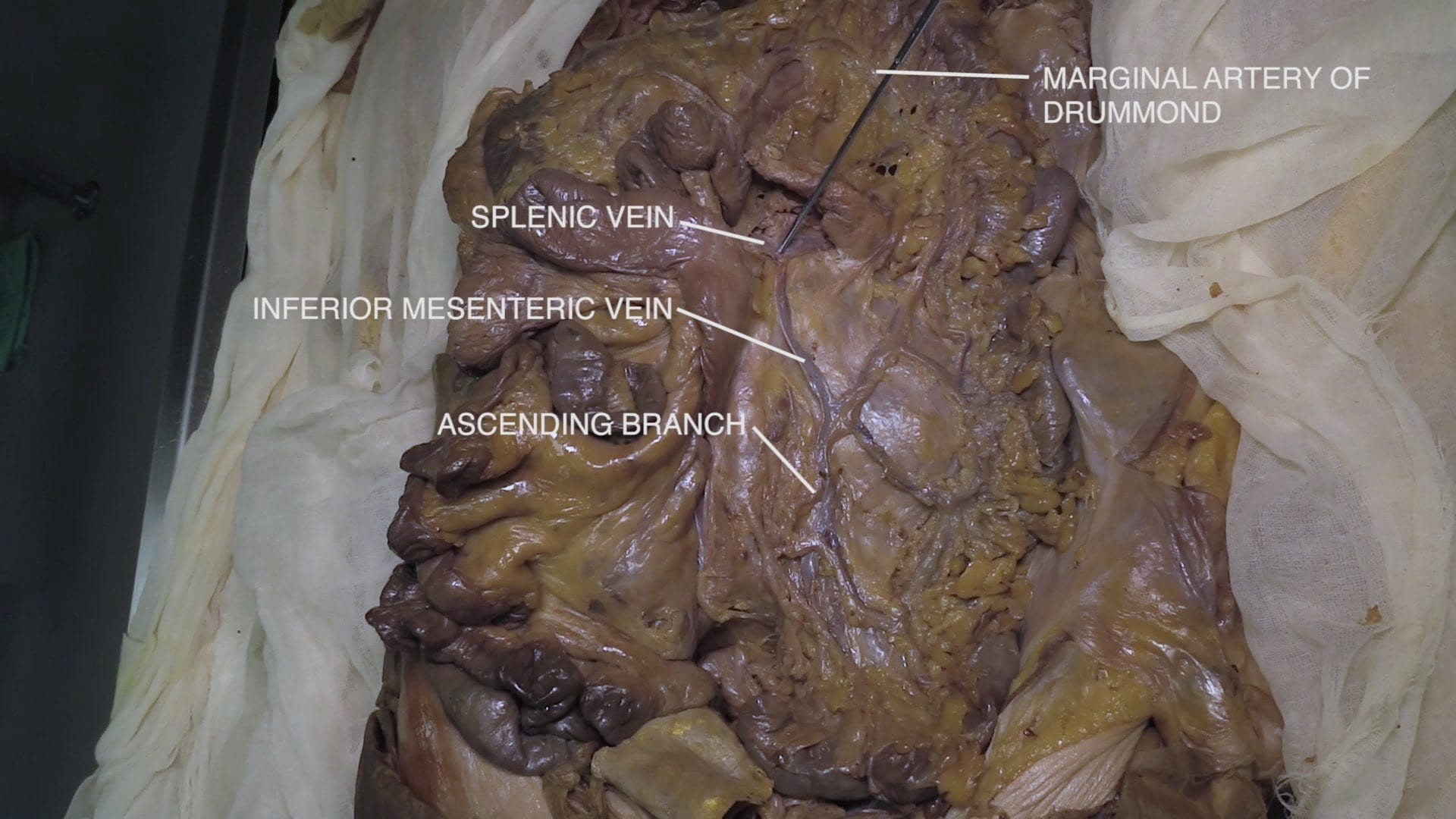
- Be able to describe the contribution of the splenic, superior mesenteric and inferior mesenteric veins to the portal system.
- Explain the functional importance of the marginal artery of Drummond.
Lecture List
Right Retroperitoneum, Left Retroperitineum, Mesenteric Vessels
Right Retroperitoneum
White Line of Toldt
Retroperitoneum
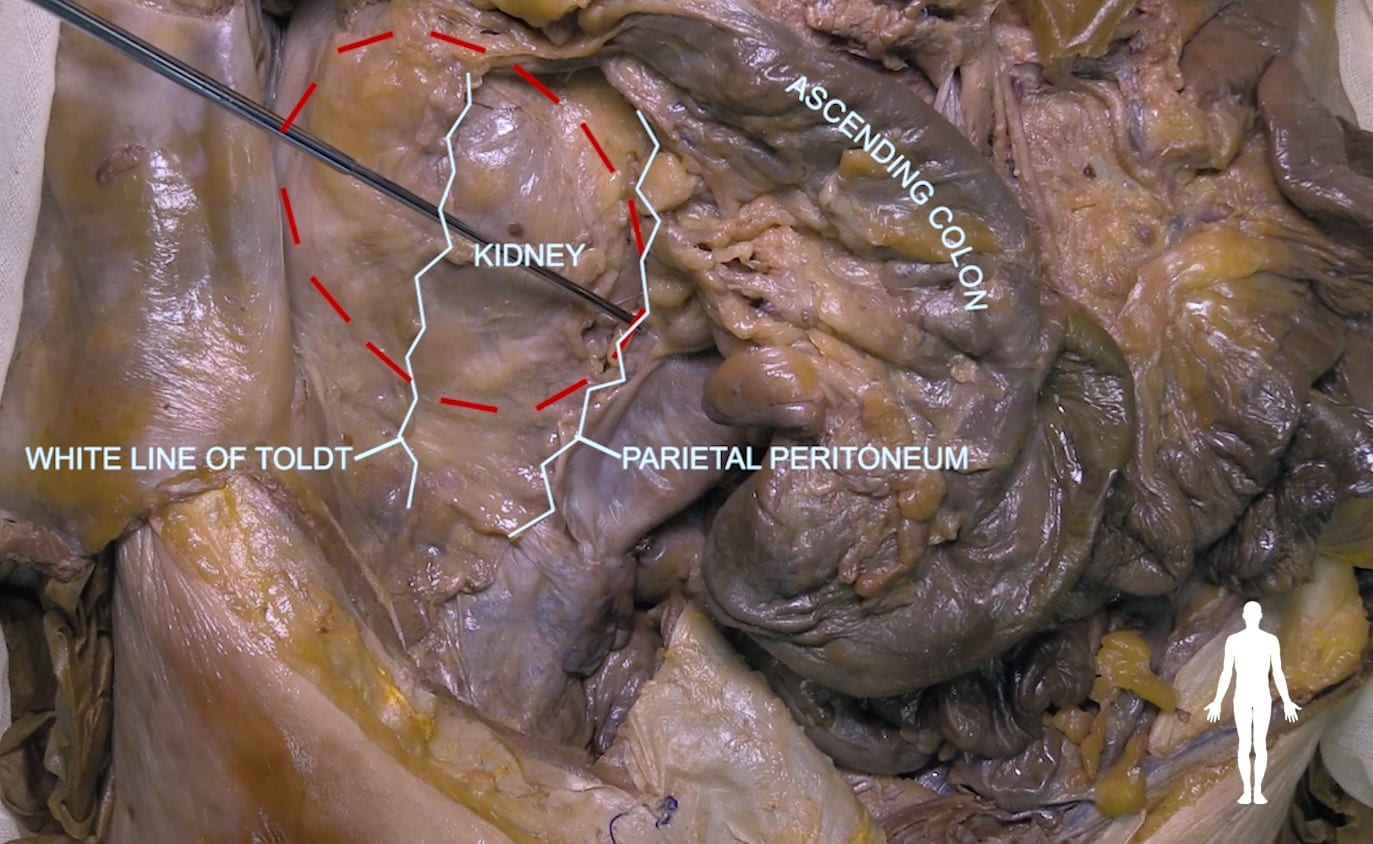
Kidney and Adrenal (Suprarenal) Exposure
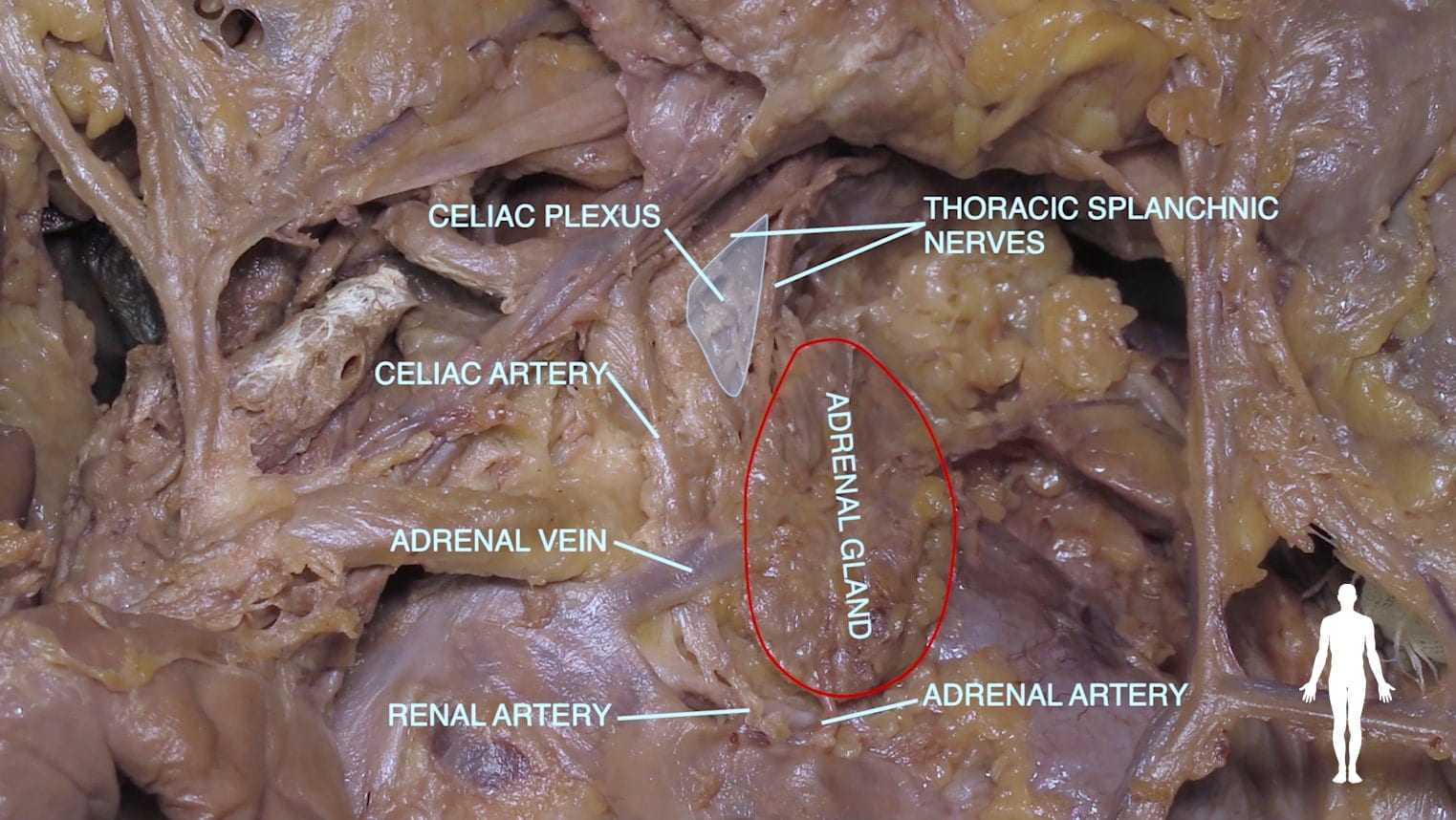
Remove the fatty tissue surrounding the kidney. This is the pararenal and perirenal fat. The adrenal (suprarenal) gland is adjacent to the upper medial pole of the kidney. Spare this portion of fat surrounding the kidney.
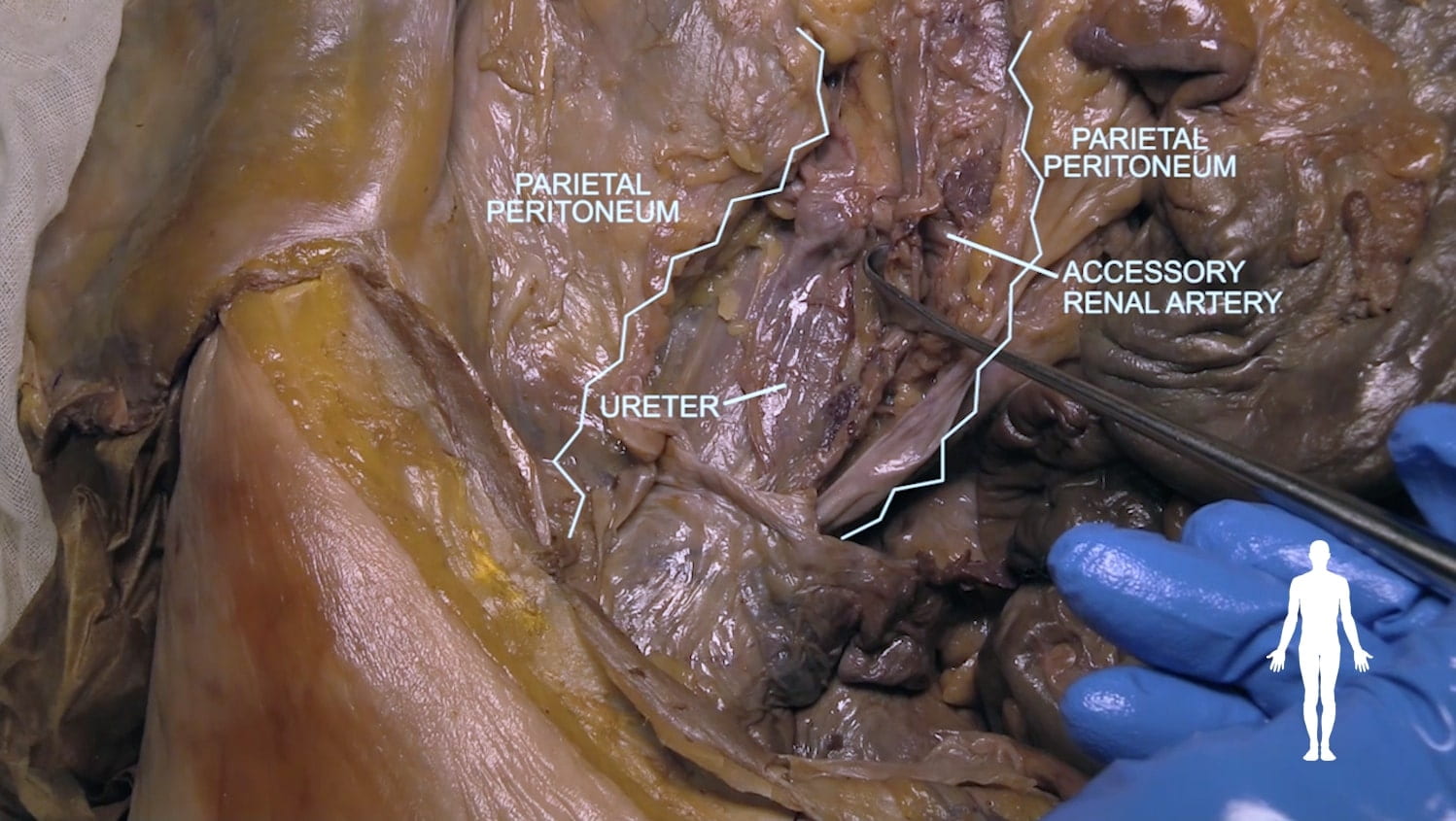
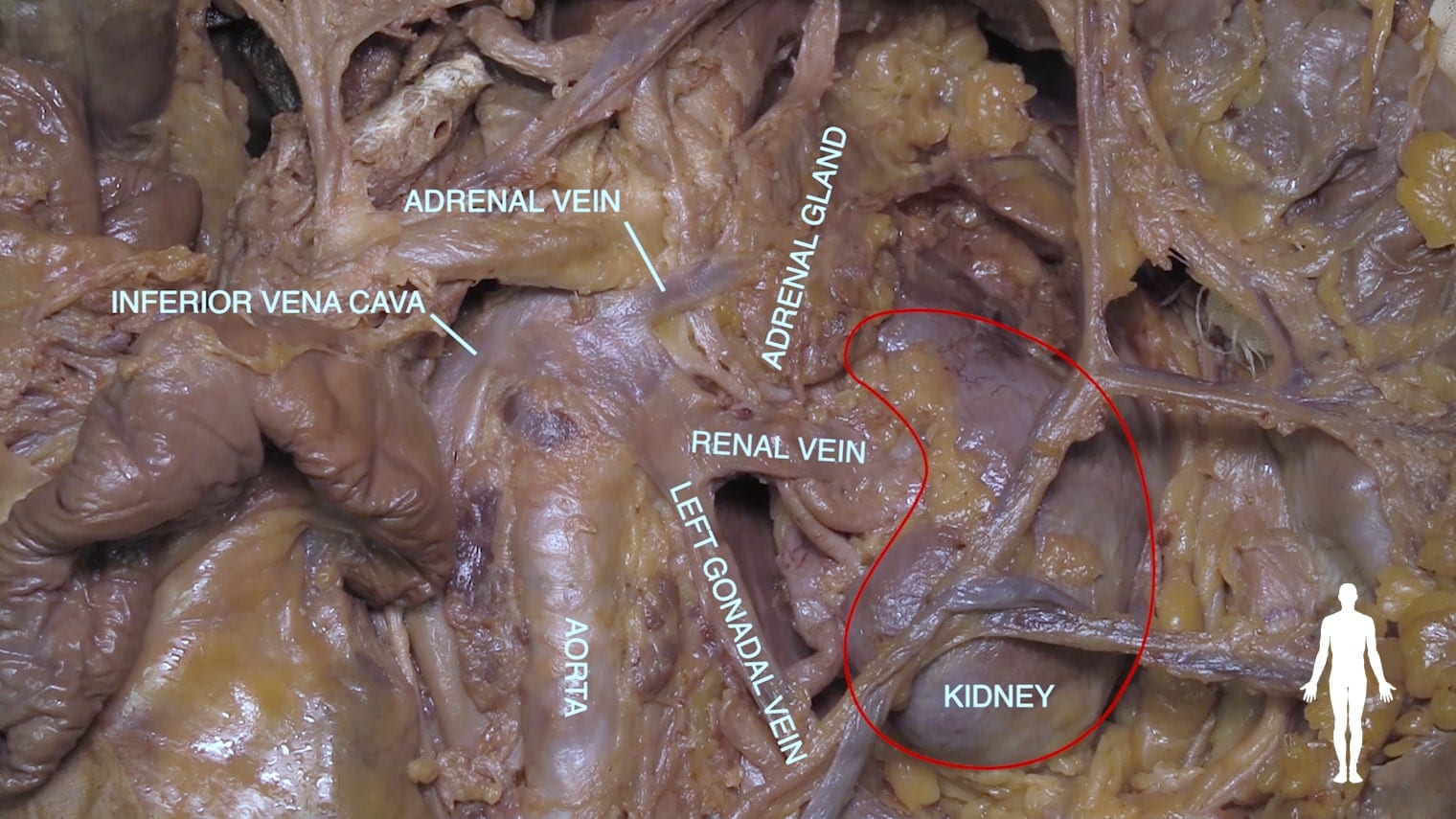
Identify the renal artery, renal vein and ureter. You may need to divide the renal vein in order to see the renal artery and ureter.
You may be able to follow adrenal vessels to the gland at this point. Locate the adrenal gland.
Note the variability of renal arterial blood supply among donors. Note the short course of the renal vein to IVC.

Kidney
Bisect the kidney into anterior and posterior halves; use a large knife.
Identify the following structures:
- Renal cortex
- Renal columns
- Renal pyramids
- Major and minor calyces
- Renal pelvis
- Ureter

Left Retroperitoneum
Descending Colon
Identify the spleen, descending colon and sigmoid colon. Mobilize the descending colon by incising along the white line of Toldt on the left side.
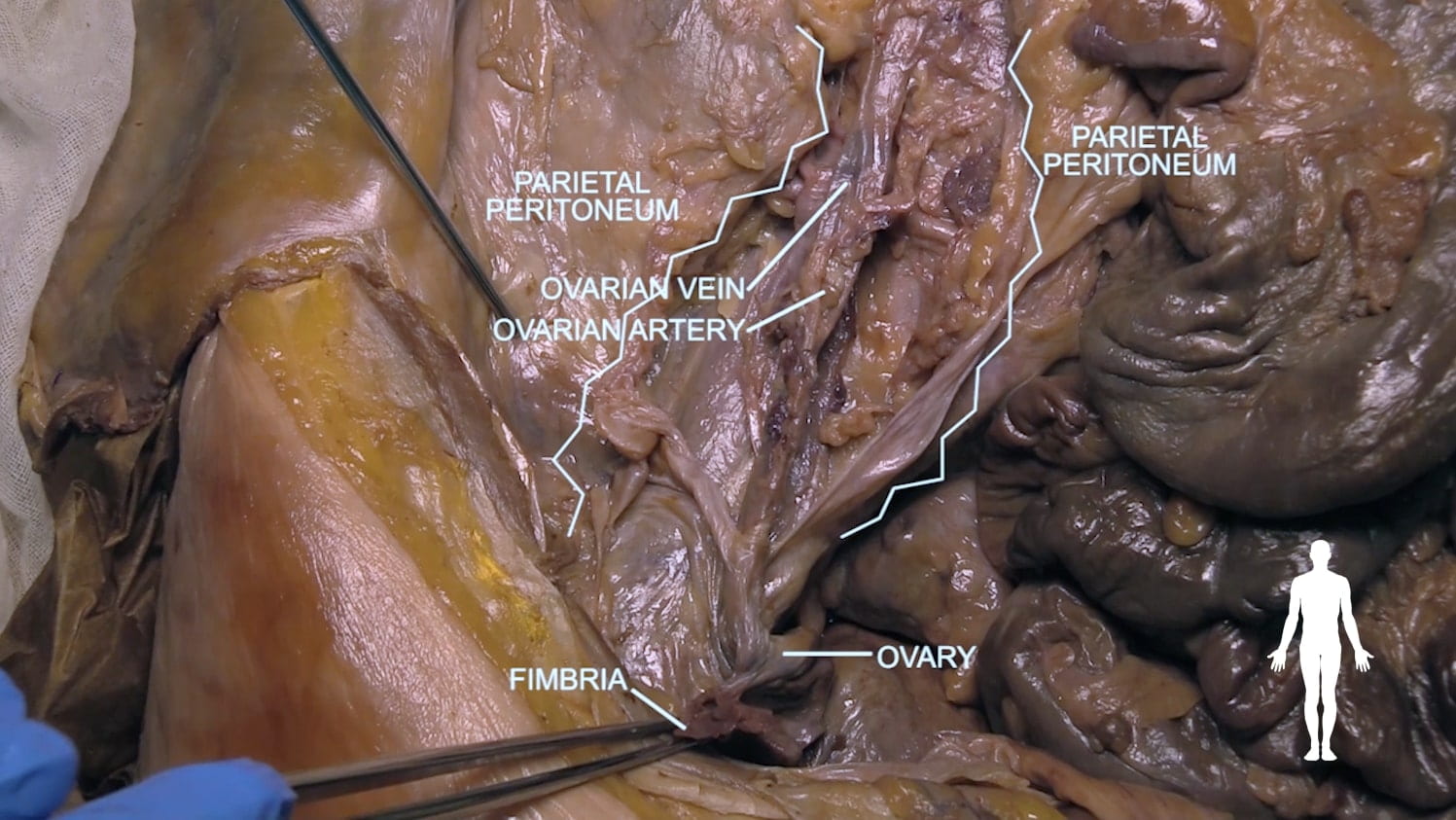
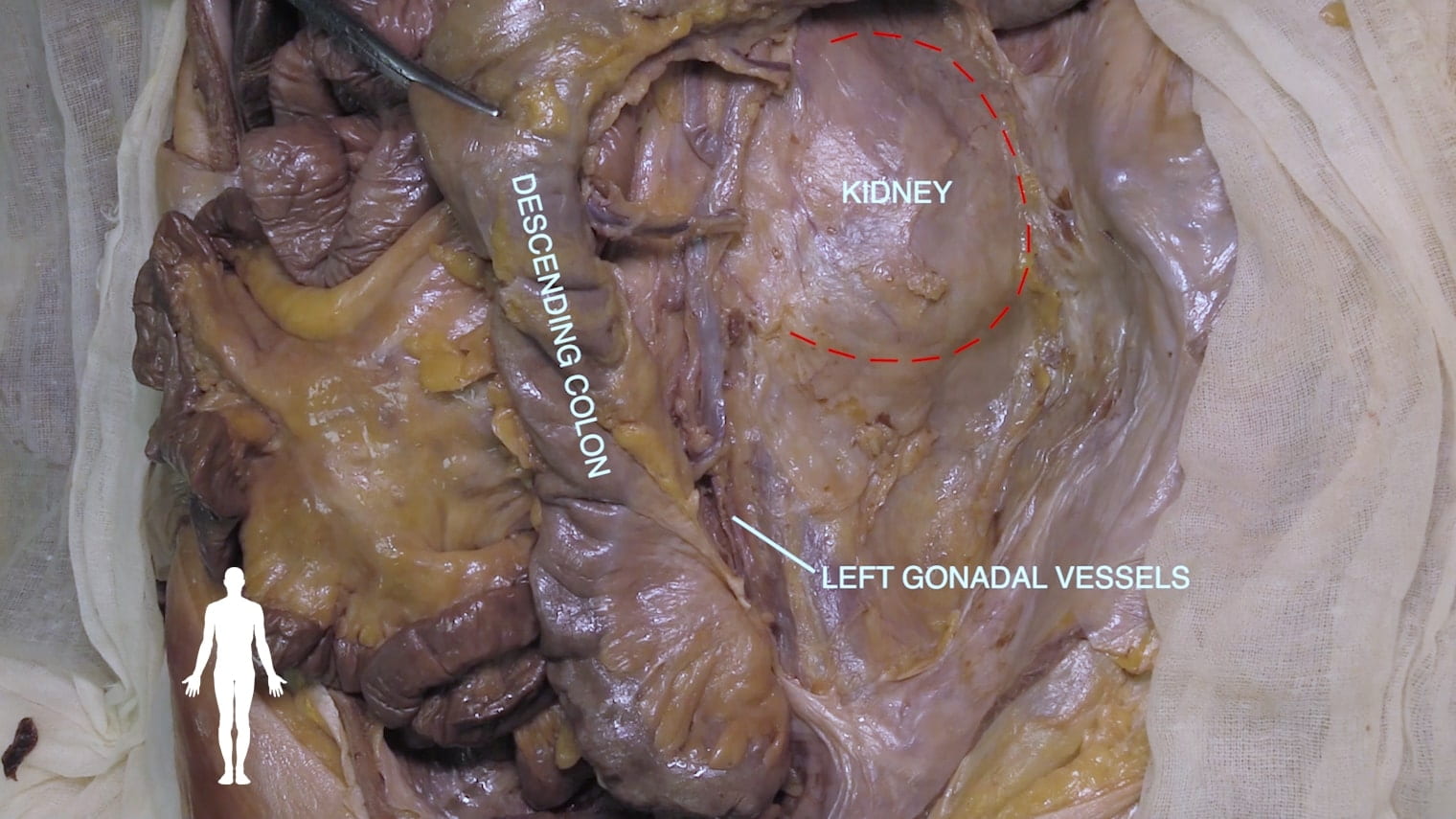
Expose the gonadal vessels on the left and locate the kidney.
Major Retroperitoneal Vasculature
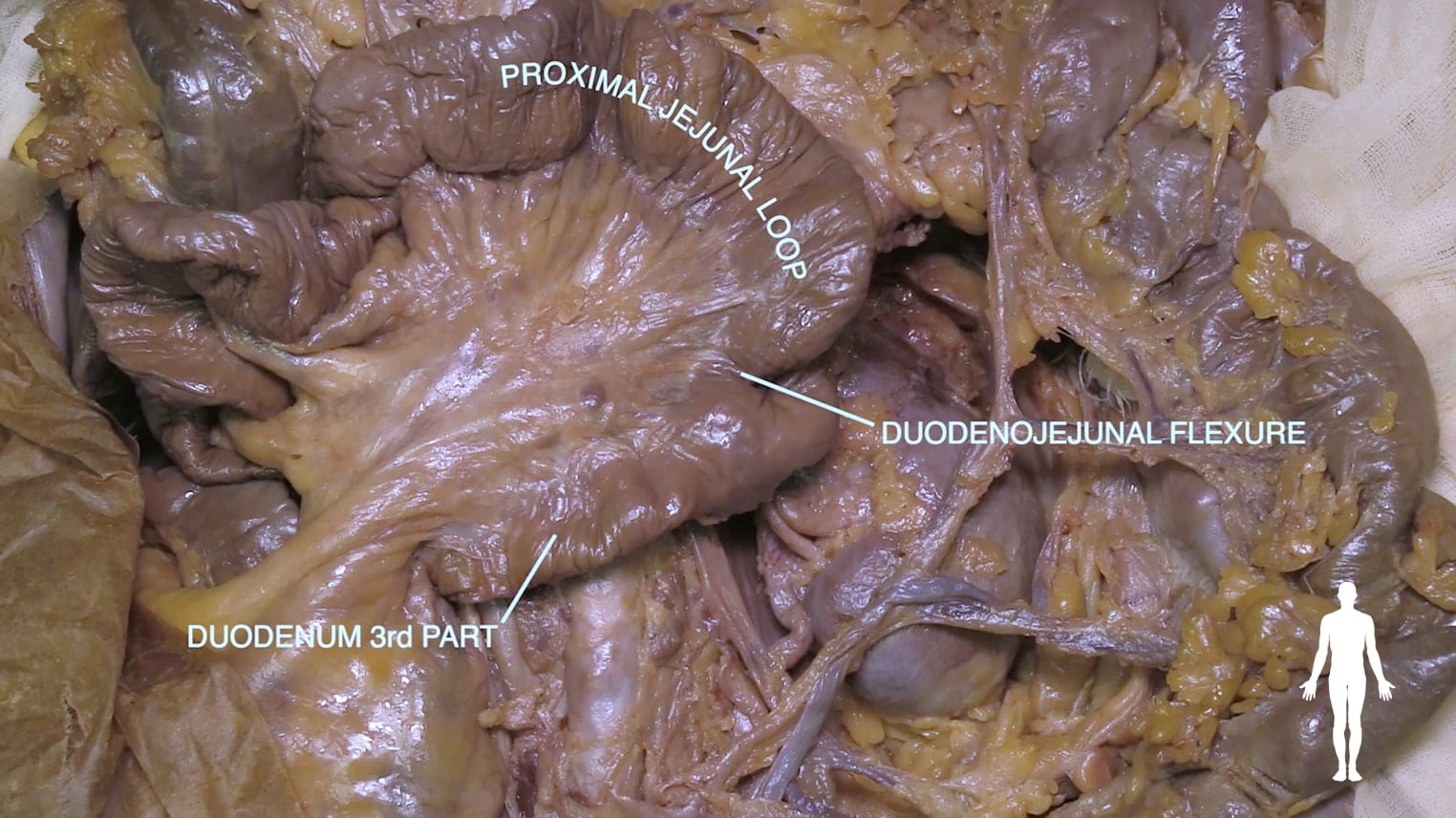
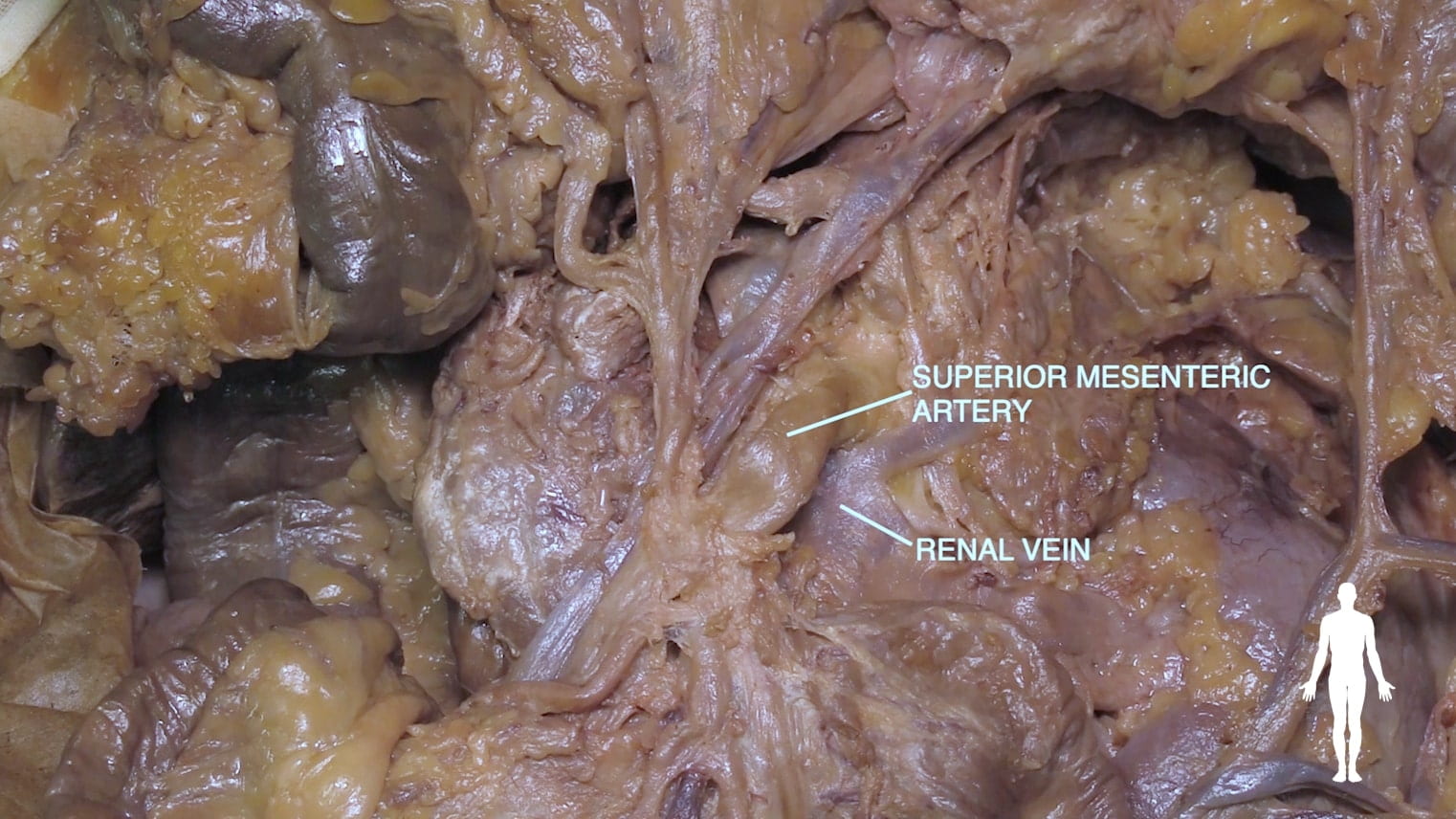
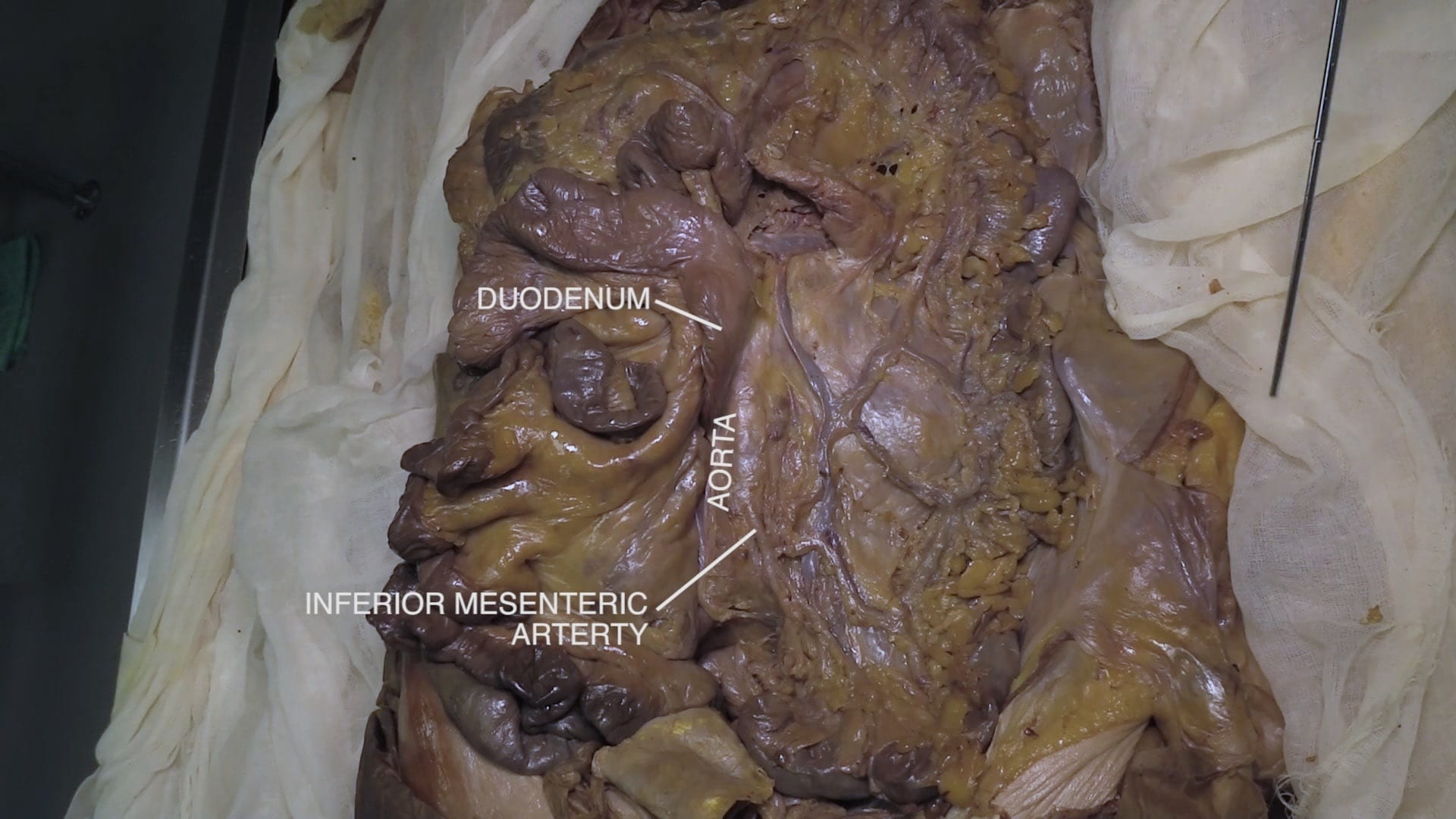
Mobilize the 3rd part of the duodenum by incising along its inferior border. Reflect the duodenum to the right.
Locate and identify the following structures posterior to the anatomic position of the 3rd portion of duodenum:
- Aorta
- IVC
- Left renal artery and vein
- Adrenal gland
- Left gonadal vein
- Kidney
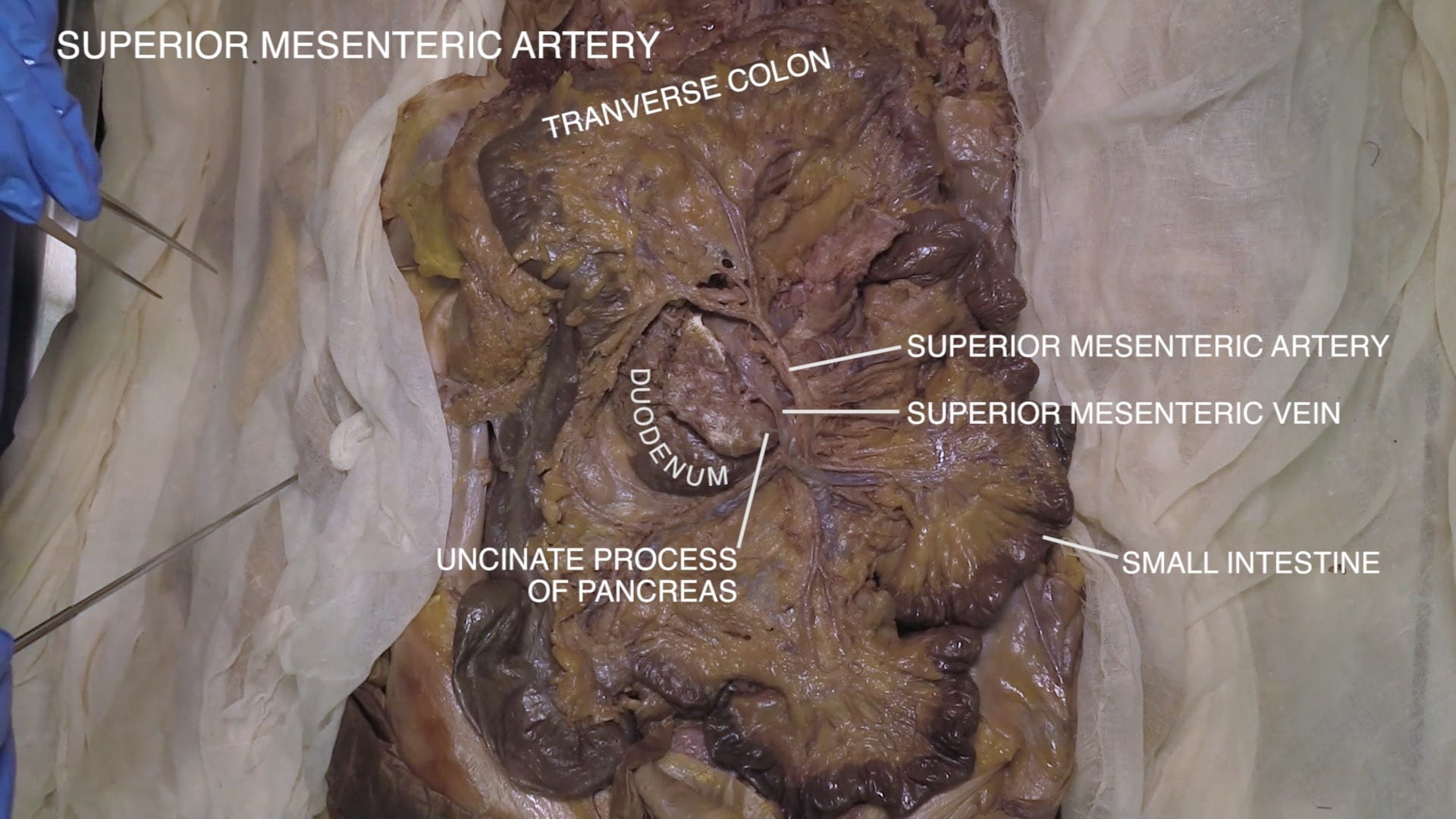
- Superior mesenteric artery and vein (SMA and SMV)
- Celiac artery
- Celiac plexus and splanchnic nerves (difficult to identify)
Superior Mesenteric Artery (SMA)
Mesenteric Vessels
Transverse Mesocolon
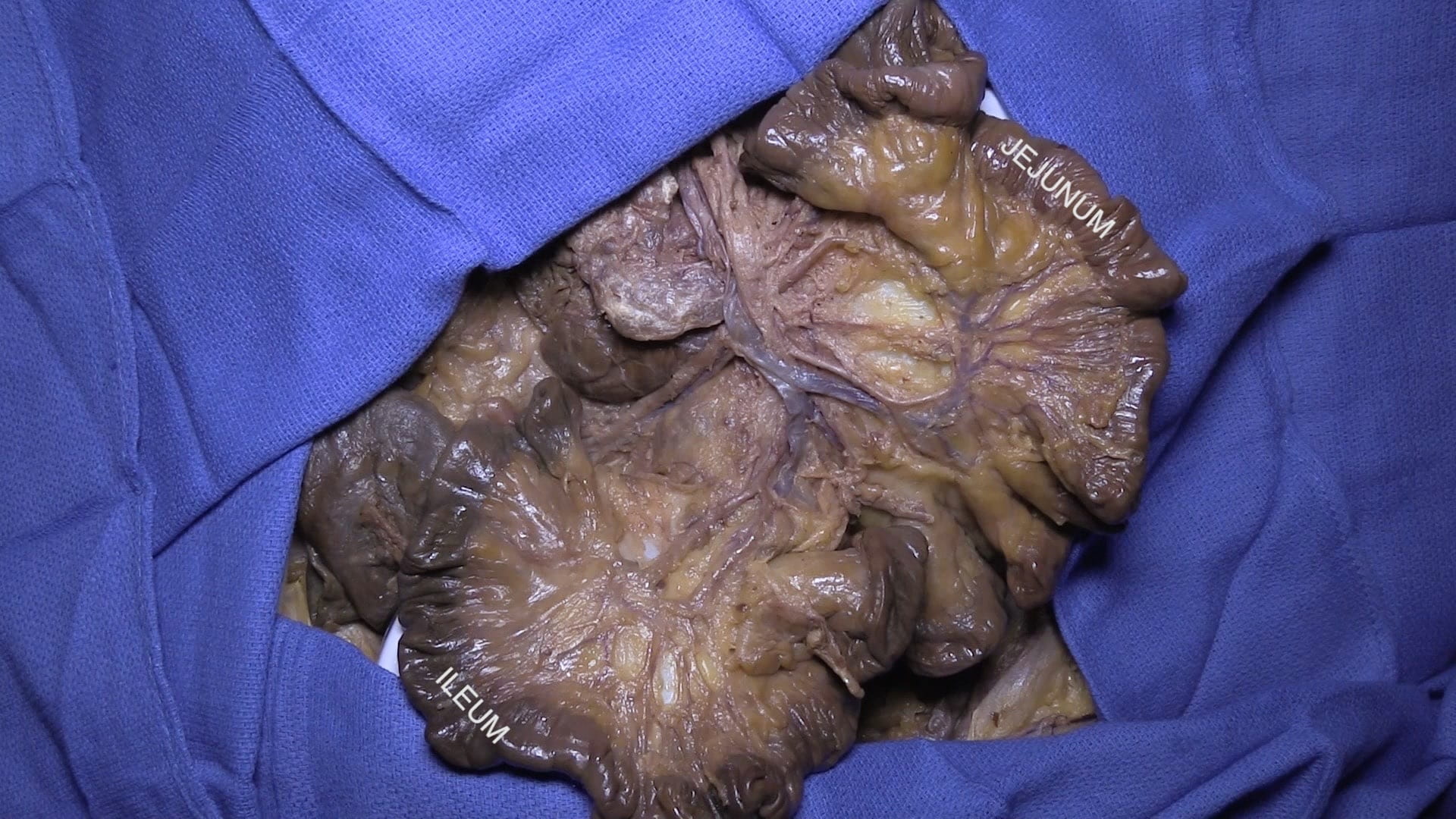
Elevate the greater omentum and locate the transverse mesocolon, i.e., the mesentery of the transverse colon. Move the small intestine laterally to identify its mesentery.
Follow the vasculature of these mesenteries. This will require blunt dissection. Some donors may have considerable fat in the mesentery that requires more extensive dissection. Note that sharp dissection is likely to damage this vasculature.

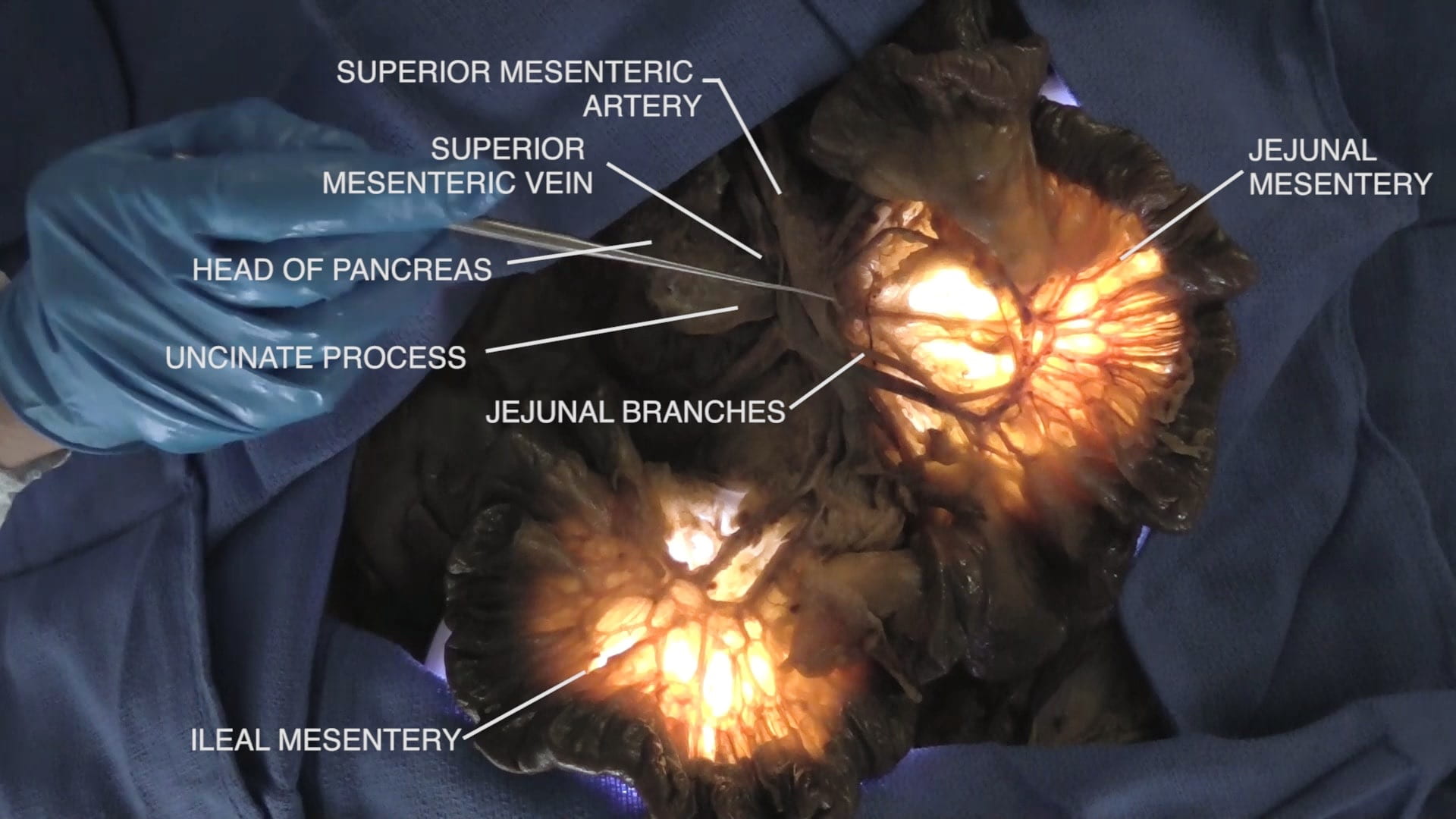
Superior Mesenteric Vasculature
Incise the neck of the pancreas and reflect its body to the left to reveal the formation of the portal vein from the superior mesenteric vein and splenic vein.
Locate the origin of the superior mesenteric artery posterior to the portal vein.
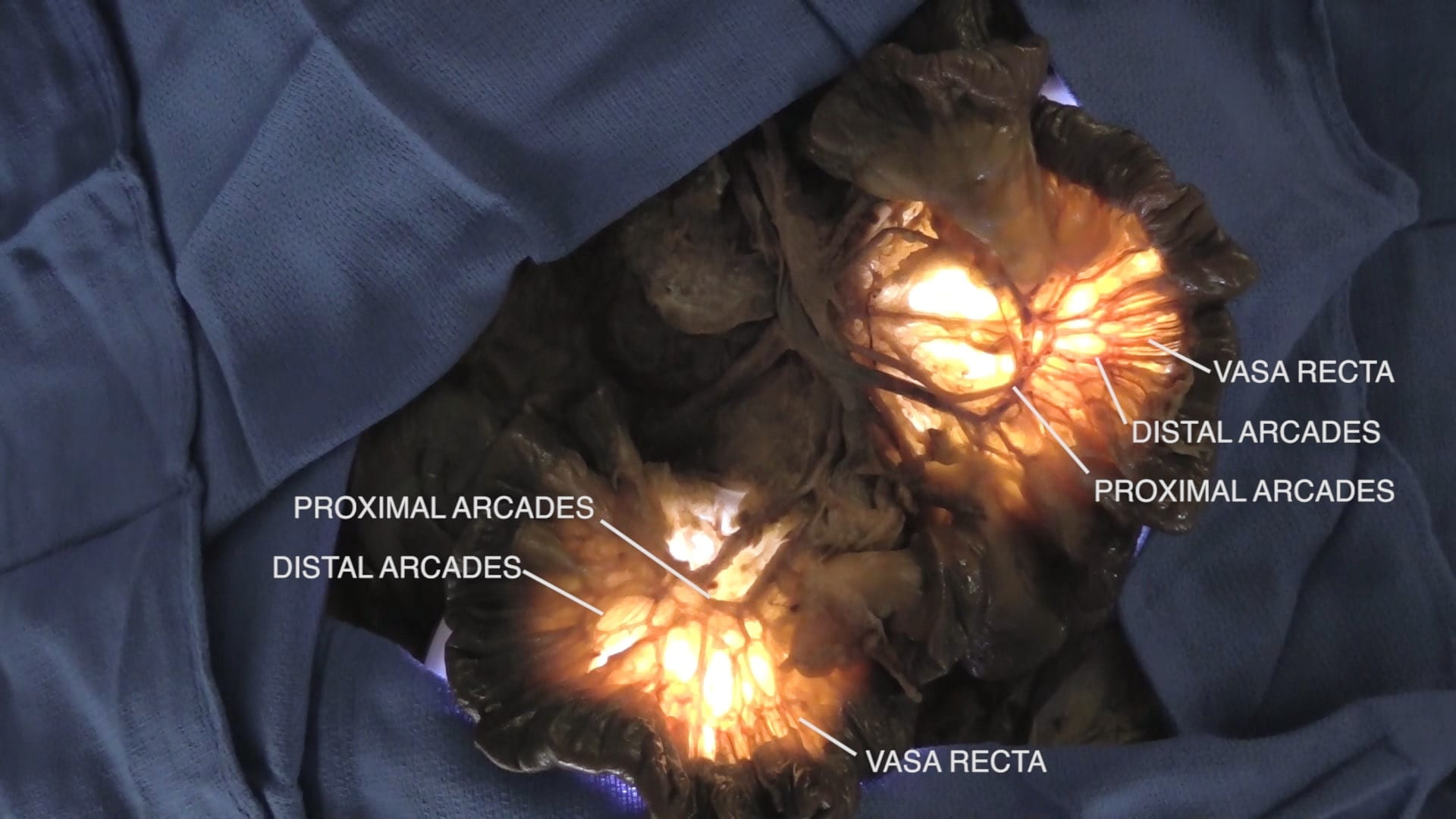
SMA Branches
Mesenteric Arcades
Bluntly dissect segments of the mesentery at proximal jejunum and distal ileum. Examine the arcades (anastomoses) between branches of the vessels and the vasa recta.
Inferior Mesenteric Artery (IMA)
Physical Examination of Abdomen
Colonoscopy, Harry Asianian
Colonoscopy – Ileum, Harry Asianian
Retroperitoneum Clinical Correlations
Trauma/EM: Retroperitoneal Hemorrhage: Retroperitoneal hemorrhage may occur secondary to trauma (blunt or penetrating injury) or non-traumatic causes (spontaneous or iatrogenic). Patients with retroperitoneal hemorrhage may present insidiously before entering hypovolemic shock due to severe blood loss. In some cases, physical exam will be significant for bruising/edema in the periumbilical and flank regions; respectively known as Cullen’s sign (tracking of hemorrhage from retroperitoneum to umbilicus along gastrohepatic and falciform ligaments) and Gray Turner’s sign (extravasation of hemorrhage across the transversalis fascia and tracking along quadratus lumborum muscle). Contrast-enhanced CT is generally diagnostic. The life-threatening bleeding associated with retroperitoneal hemorrhage must be rapidly accessed for identification of bleed origin and management. Anterior access to the retroperitoneum is relatively complex and time-consuming due to the intervening intraperitoneal organs and mesentery. Instead, quick access to the retroperitoneum is generally achieved through left or right medial visceral rotation. Recall that the ascending and descending colon are anchored to the lateral body wall: the point where the visceral peritoneum of the colon meets the parietal peritoneum of the body wall is the white line of Toldt (make sure to see this in lab!). Incision of this creates the dissection plane into the retroperitoneum that is continued just superficial to the posterior abdominal muscles. As the dissection plane is developed, various organs (i.e., the viscera) including the kidneys, ureters, ascending or descending colon are medially rotated. This can be done on the left (the Mattox maneuver) for access to the aorta or the right (the Cattel-Braasch maneuver) for access to the IVC. The Mattox maneuver generally involves rotation of the stomach, spleen, and pancreas as well. See image below for visualization of procedure.
Procedure: Celiac Plexus Block: The celiac plexus are the bundles of nerves located around the celiac trunk, SMA, renal arteries branching off the aorta. This plexus is formed by the greater and lesser splanchnic nerves (sympathetic) and the branches of the vagal trunk (parasympathetic). Functionally, these nerves regulate physiological function of and blood flow to many abdominal organs. Additionally, the celiac plexus transmits pain signals from the abdominal viscera to the central nervous system. As a result, the celiac plexus is a key target in pain management strategies for patient’s suffering from intractable abdominal pain caused by malignancy (e.g., pancreatic) and pancreatitis. Block is classically achieved through injection of an anesthetic or neurolytic agent (choice depends upon etiology of pain) into the celiac plexus. Access to the celiac plexus is achieved through an anterior or posterior para-aortic approach under image guidance. Anterior approach generally involves transversing bowel and liver. The posterior approach entails insertion of the needle through paraspinous musculature.
Embryology: Horseshoe Kidney: The embryological development of the kidneys is multi-staged and complex. Horseshoe kidney occurs when the primitive kidneys fuse at their lower poles; this point of fusion is the isthmus. In addition to this abnormal isthmus, horseshoe kidneys generally differ from normal kidneys in their location and vasculature. Primitive kidneys begin development low in the abdomen before ascending. In the case of horseshoe kidney, the isthmus can be “caught” by the origin of vasculature (e.g., IMA) coming off the aorta thus impeding normal ascent. Vasculature of the horseshoe kidney can be highly variable with multiple renal arteries from the aorta/iliac vessels and aberrant veins. Horseshoe kidney is generally asymptomatic and incidentally discovered. If symptomatic, presenting signs are generally non-specific and imaging is diagnostic. We have a horseshoe kidney in lab; ask to see it!
Surgery/Autopsy: Kidney Transplant: In patients who are functionally anephric, dialysis is used to perform many of the kidney’s filter functions. However, dialysis cannot completely substitute for physiologic kidney function thus outcomes for dialysis patients tend to be poor. For this reason, dialysis is best viewed as a bridge to renal transplant (when possible). Think: are the patient’s native kidneys removed? No! Recall that the kidneys are retroperitoneal and receive ~25% of the cardiac output: access and removal of these would be time-consuming and operatively complex in patients who are severely ill to begin with. Removal of native kidneys is considered in cases of severe infection (pyelonephritis) or severe renal enlargement (e.g., polycystic kidney disease). Now, what about the donor kidney- where is it placed and how is it vascularized? Again, to avoid complicated access to the retroperitoneum, the new kidney is generally implanted in the right iliac fossa (lower right abdomen) and connected to the iliac vessels. If you see a kidney recipient, palpation of the kidney graft in this region is typical during physical exam. On a separate note, ask about innervation of the donated kidney in lab!
Anatomical Variations: IVC Variations: During development, there is a complex system of left- and right-sided embryological veins that ultimately fuse and regress to give rise to the mature caval system. If this process goes awry, IVC variations develop. Persistence of an embryological cardinal vein can give rise to a duplicated IVC. If the right-sided embryological veins inappropriately regress and left-sided ones persist, a left-sided IVC develops. In some cases, the infrarenal IVC (i.e., below the kidney) can be entirely missing. Though rare, these variants are important to identify prior to operations such as abdominal aortic aneurysm repair, nephrectomy, and IVC filter placement.
Imaging: Multimodality imaging is utilized for evaluating the kidneys and collecting systems. Ultrasound is a preferred starting modality for evaluating hydronephrosis or renal calculi (or for evaluating pediatric kidneys), but the ureters are often difficult to image on ultrasound. CT of the abdomen and pelvis without contrast is the workhorse for evaluating concern for renal calculi causing renal/ureteral obstruction. CT with intravenous contrast can be used for better imaging of the renal parenchyma and looking for infection, tumors or suspected injury. CT urography involves taking CT images many minutes after contrast has been injected, allowing for renal excretion of contrast into the collecting systems, ureters and bladder. This allows for evaluation of tumors, injuries or other abnormalities in these areas. MRI of the kidneys is a great way to further characterize kidney tumors or to monitor for tumor recurrence, for example after a partial nephrectomy for renal cell cancer. MRI urography can also be used for evaluating the collecting systems, with the same principles utilized as CT. CT and MRI are both used for evaluating lesions of the adrenal glands.
Images (Click to Enlarge)
Autopsy images of patient with retroperitoneal hemorrhage. Top Left) Blood visible behind peritoneum but not inside peritoneal cavity. Top Right) Retroperitoneal blood tracking along small bowel mesentery. Bottom Left) Blood dissecting along falciform ligament (red allow; mechanism of Cullen’s sign). Bottom Right) Flank hematoma (Grey Turner’s sign)




Autopsy images showing horseshoe kidney. Left: Posterior view with aorta midline. Right: Posterior view with distal aorta reflected upwards.