Duodenum and Pancreas
Lab Summary
This lab teaches the structure of the upper abdomen including proximal and distal courses of the contents of hepatoduodenal ligament, celiac trunk, duodenum and pancreas.
Lab Objectives
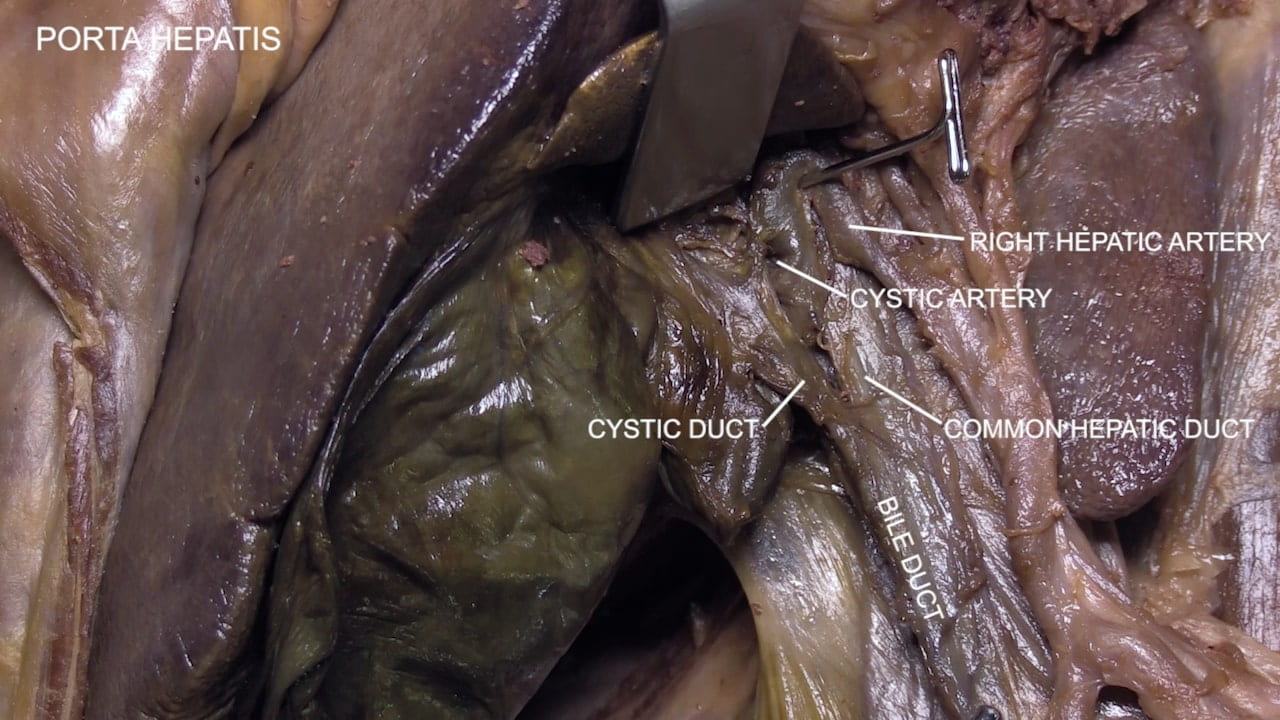
- Describe the hepatoduodenal ligament and its contents.
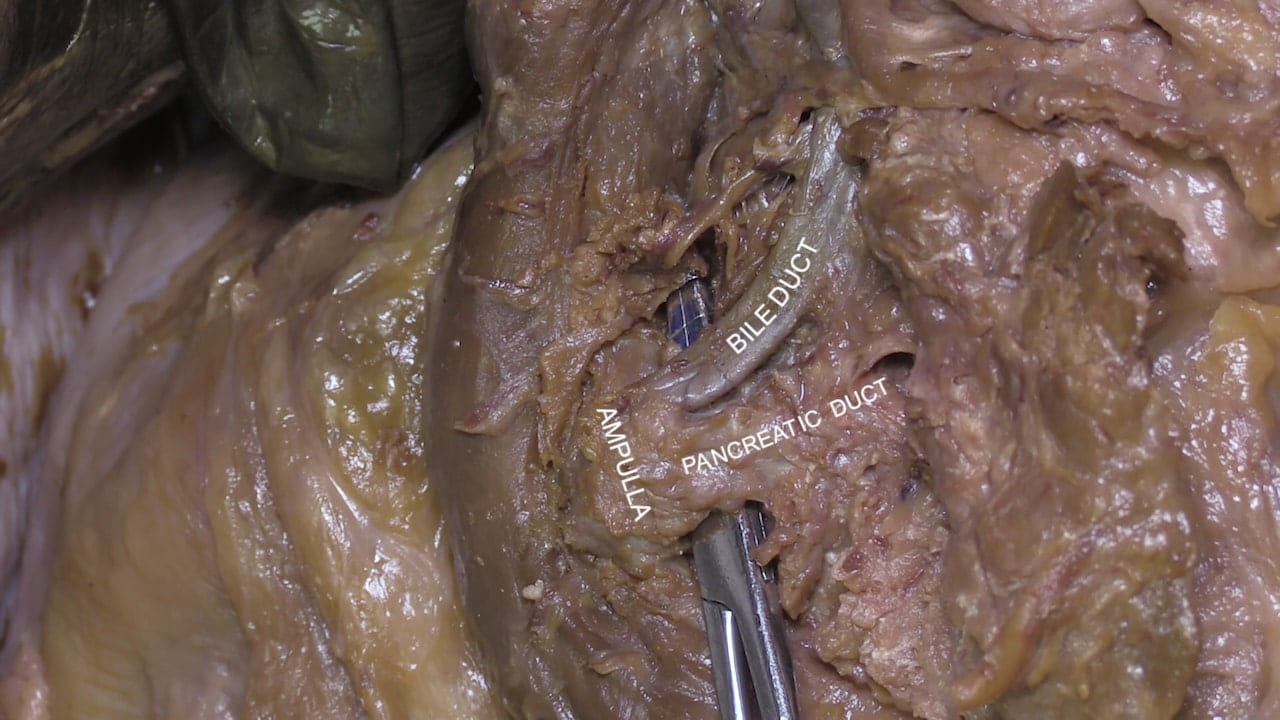
- Describe the course of the bile duct from the liver to the duodenum.
- Describe the relationship of the bile duct and the main pancreatic duct.
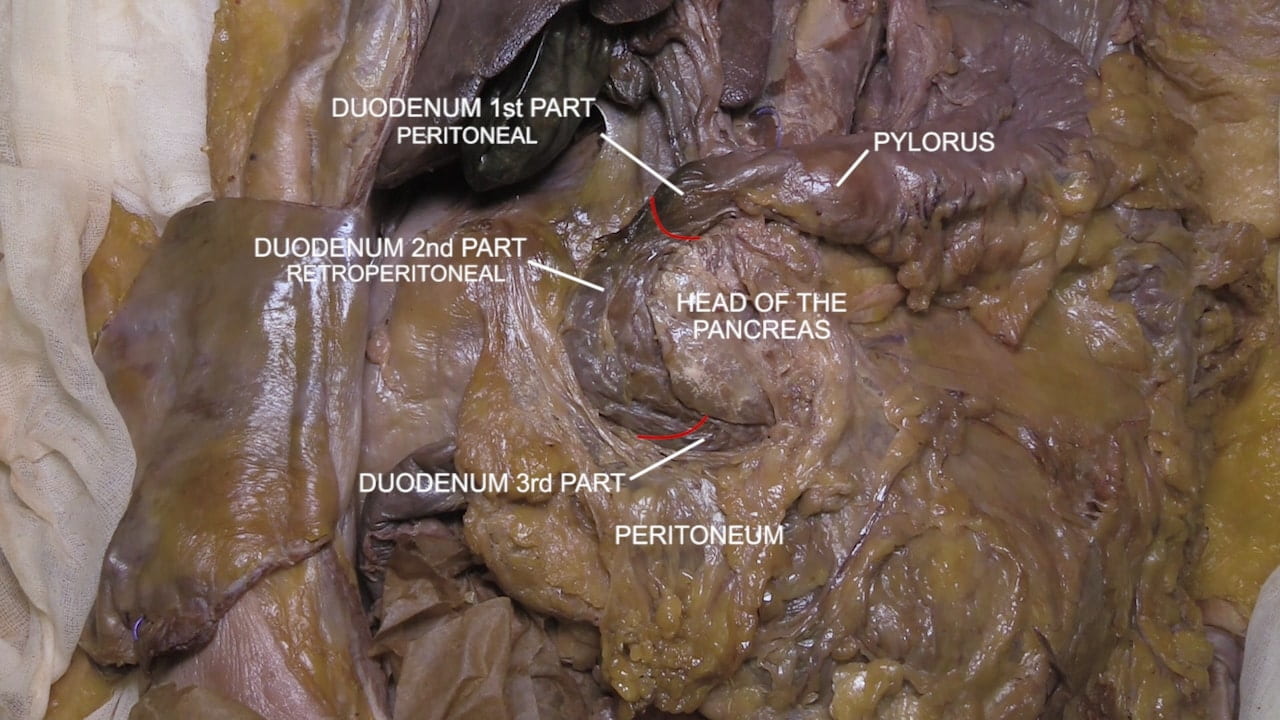
- Describe the course and relations of the parts of the duodenum.
- Name the branches and distribution of the celiac artery.
- Describe the location and relationships of pancreas to duodenum, lesser peritoneal sac and spleen.
- Describe the principal vessels ligated to remove the duodenum and head of the pancreas in a Whipple Procedure.
Lecture List
Upper Abdomen, Duodenum and Pancreas
Upper Abdomen
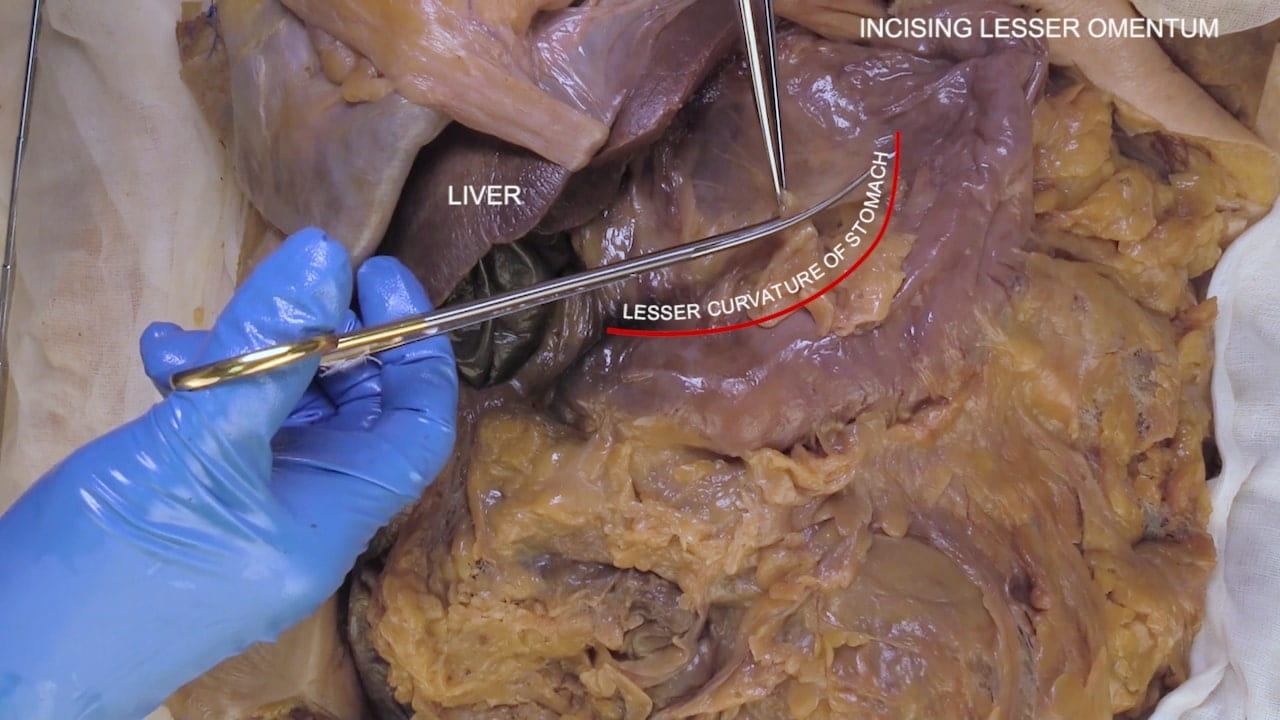
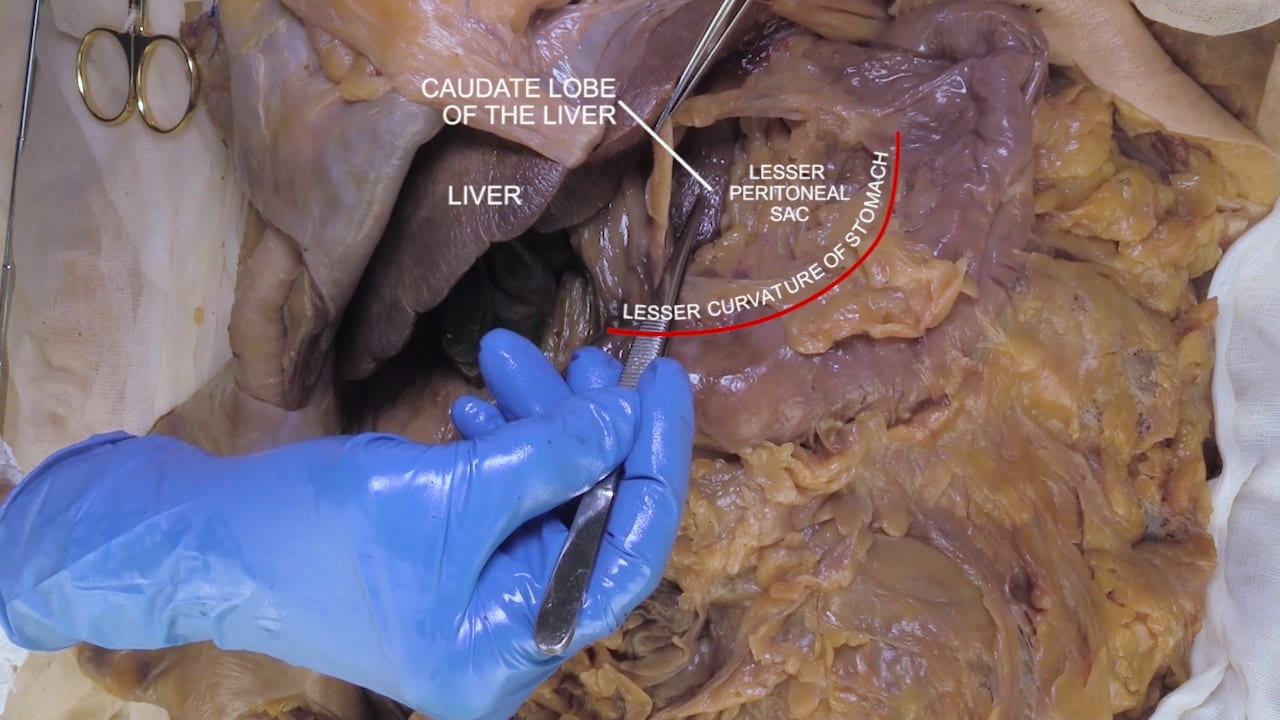
Lesser Peritoneal Sac
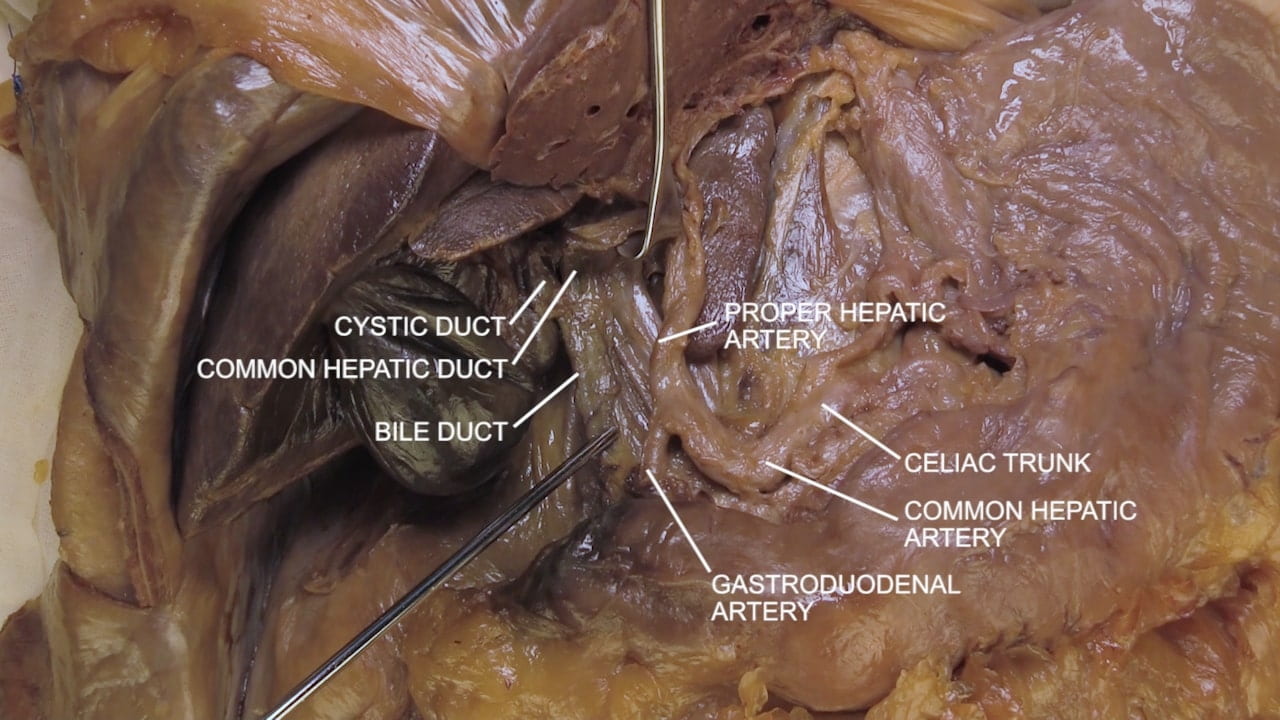
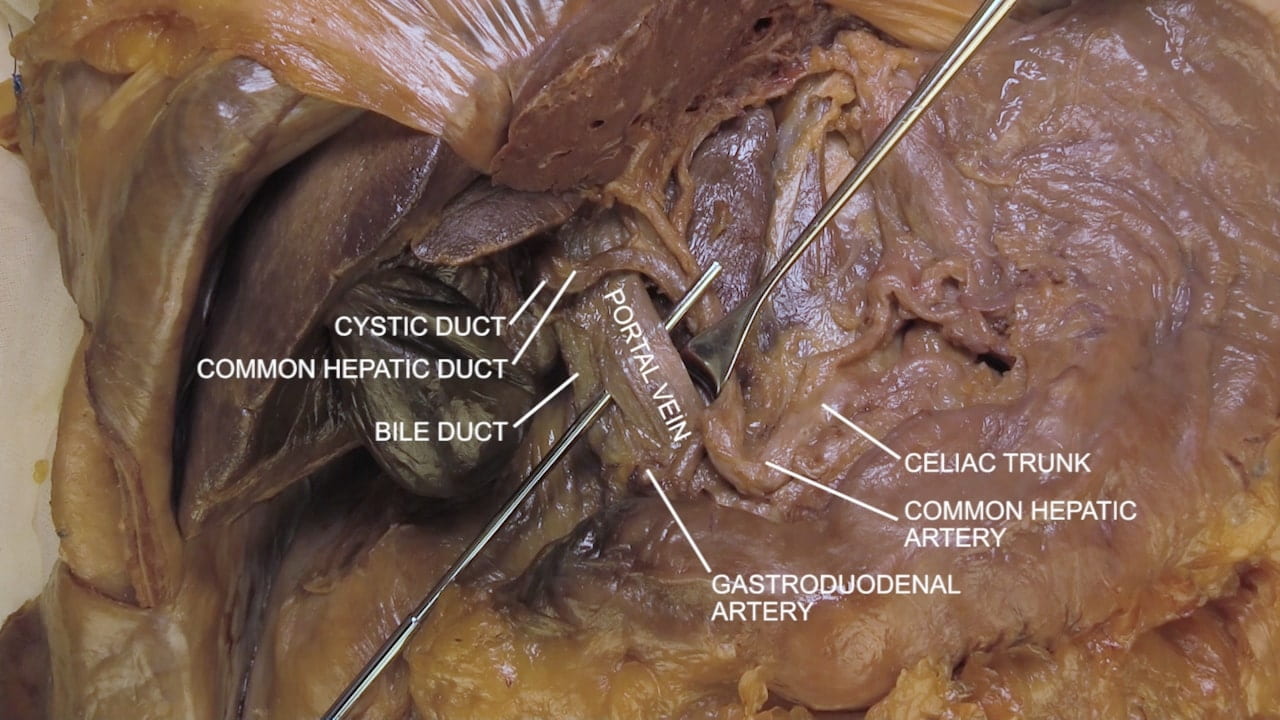
Hepatic Triad
Common Hepatic Artery
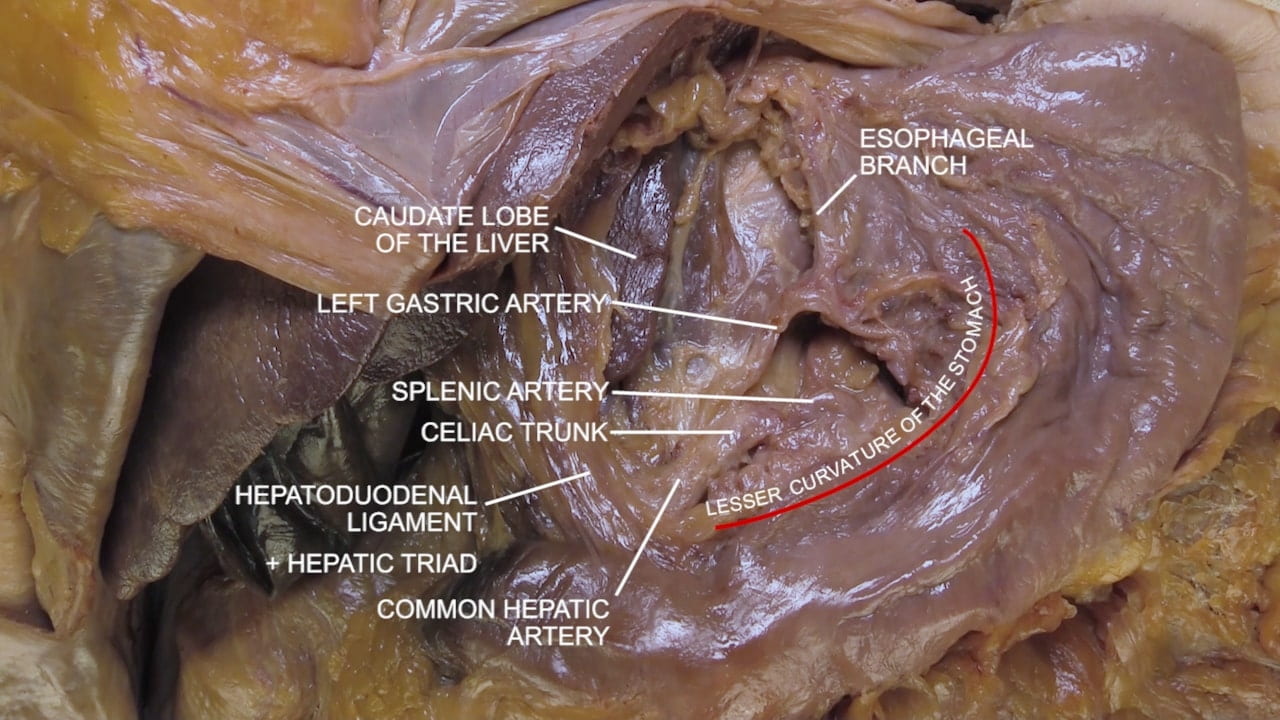
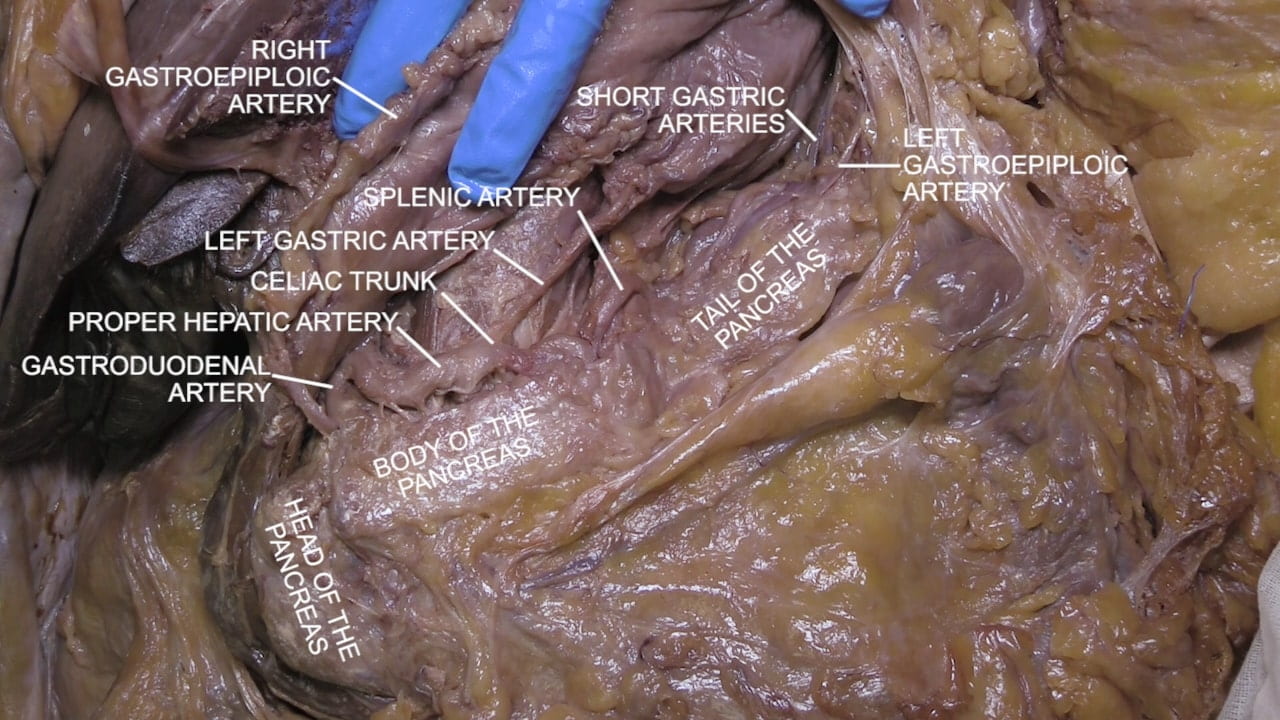
Follow the proper hepatic artery proximally to identify the celiac trunk.
Locate the left gastric artery along the upper part of the lesser curvature of stomach and follow it to the celiac trunk.
Blunt dissect through the pancreas close to the celiac trunk to locate the tortuous splenic artery.

Gastroesophageal Junction
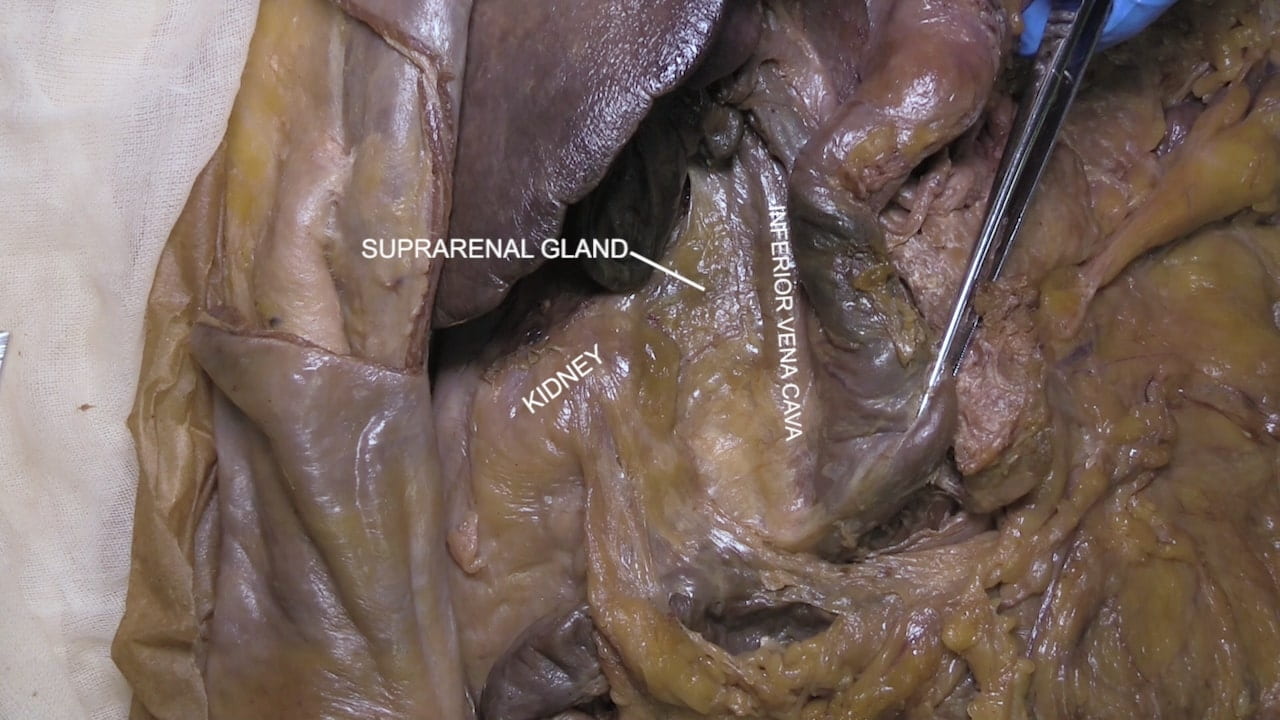
Identify the IVC above and below the diaphragm and note its close relationship to the caudate lobe of the liver.
Place an instrument in the esophageal hiatus and divide the central tendon of the diaphragm.
Identify the esophagus, gastroesophageal junction and the stomach.

Duodenum and Pancreas
Duodenum and Pancreas
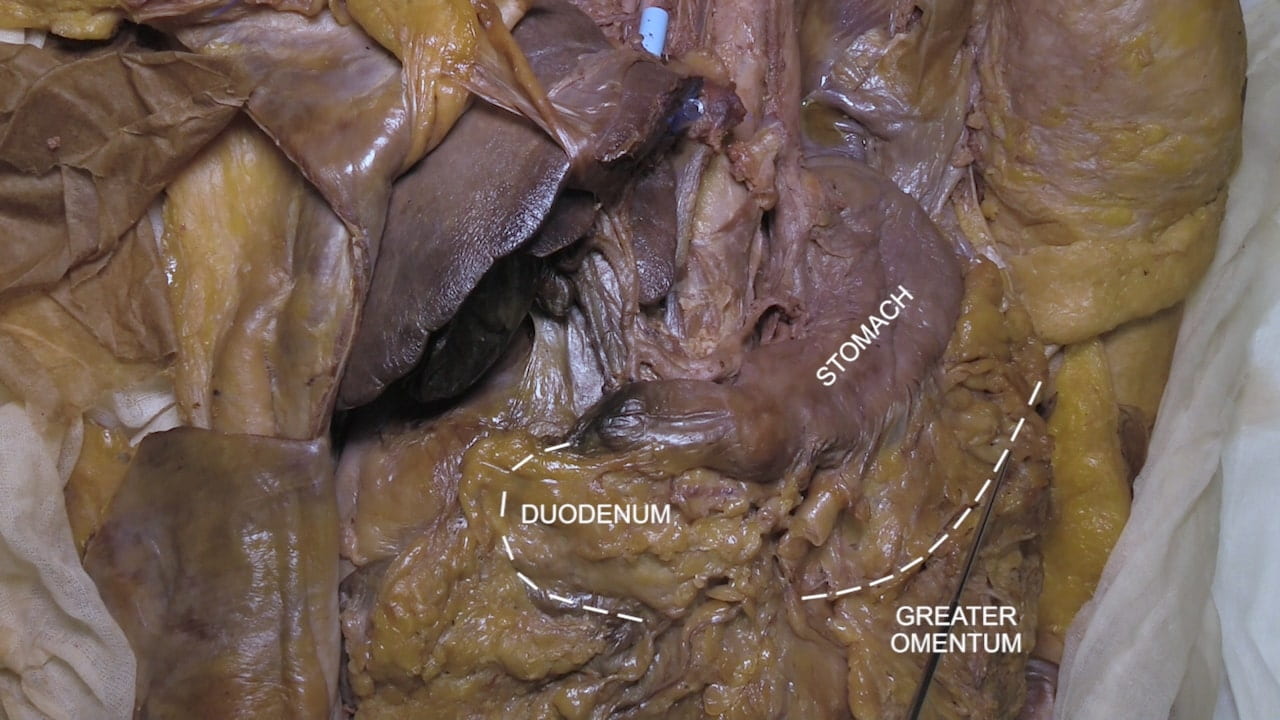
Incise the greater omentum along the greater curvature of the stomach in order to mobilize the stomach and expose the duodenum and pancreas.
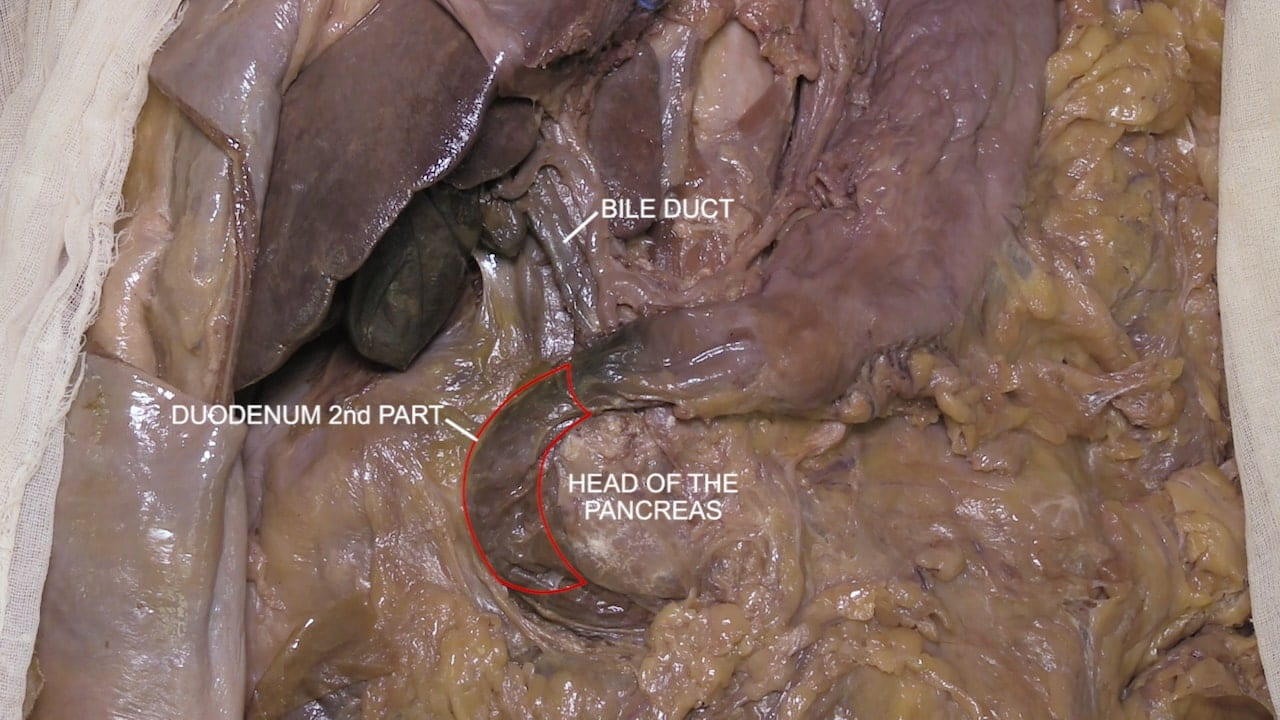
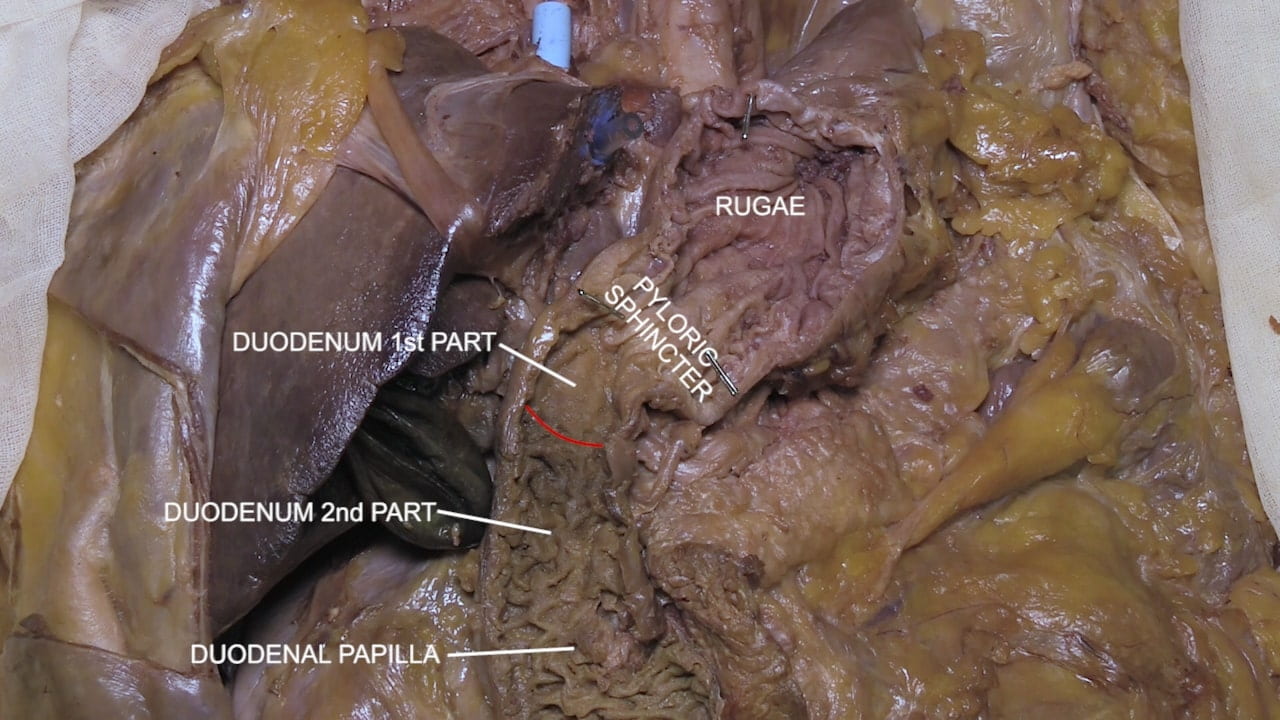
Identify the pylorus, 1st, 2nd and 3rd parts of the duodenum and the head of the pancreas. Examine the head, body and tail of the pancreas.
Identify the gastroduodenal artery as it branches from the common hepatic artery.
Bile and Pancreatic Ducts
Duodenal Papilla
Spleen
Re-identify the splenic artery and follow its course through the pancreas to the spleen. Note the splenic hilum and its close relationship to the tail of the pancreas.
Note the relationships of the spleen to 9th, 10th and 11th ribs on the left, and diaphragm, colon and kidney.

Portal Vein
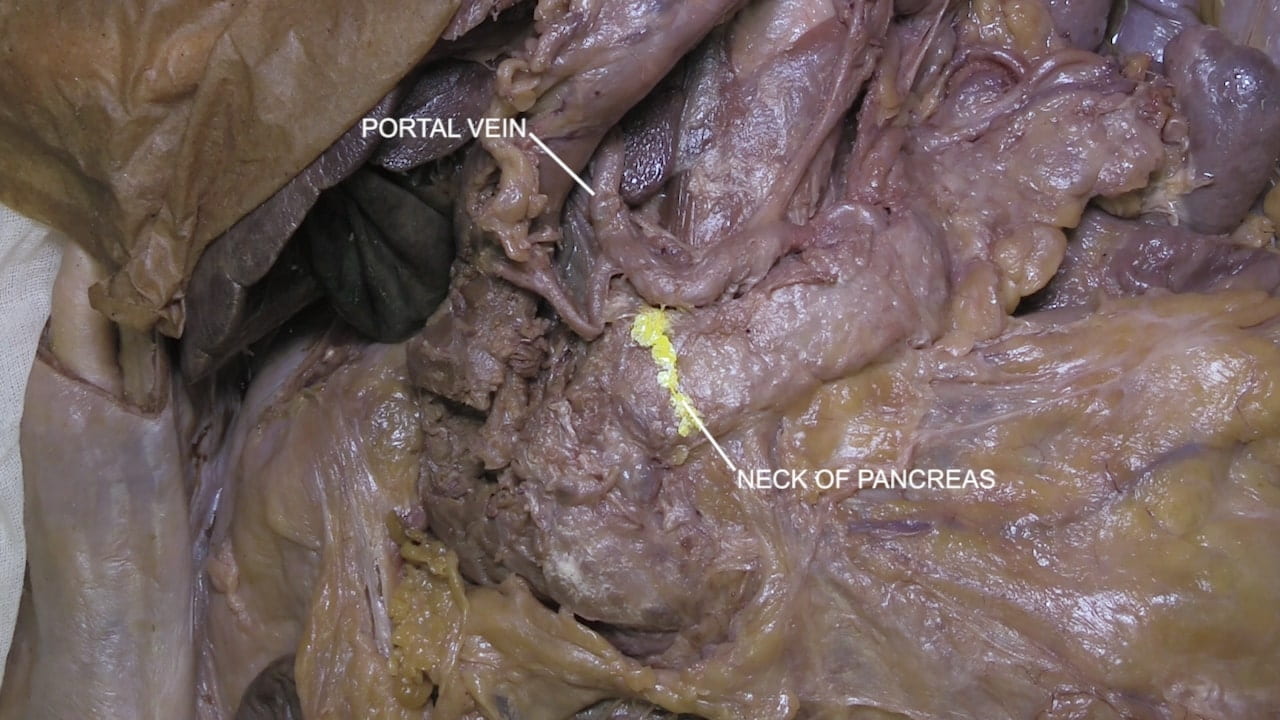
Re-identify the portal vein in the hepatoduodenal ligament.
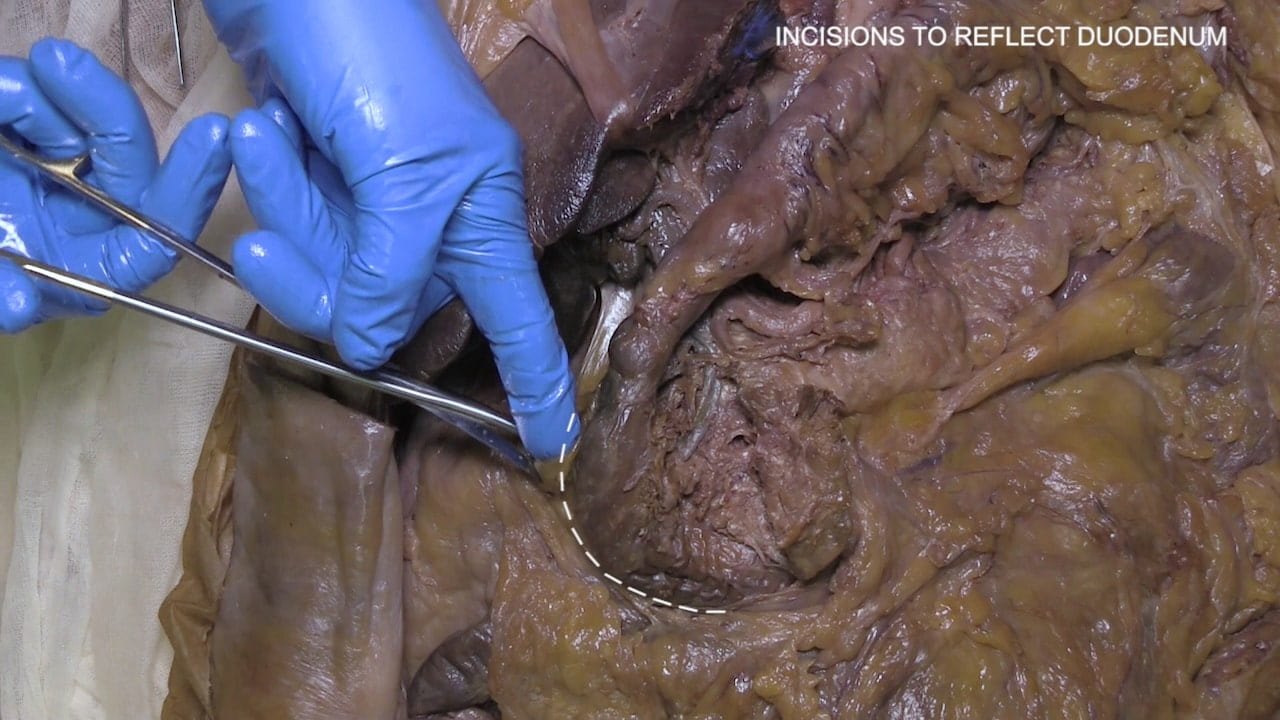
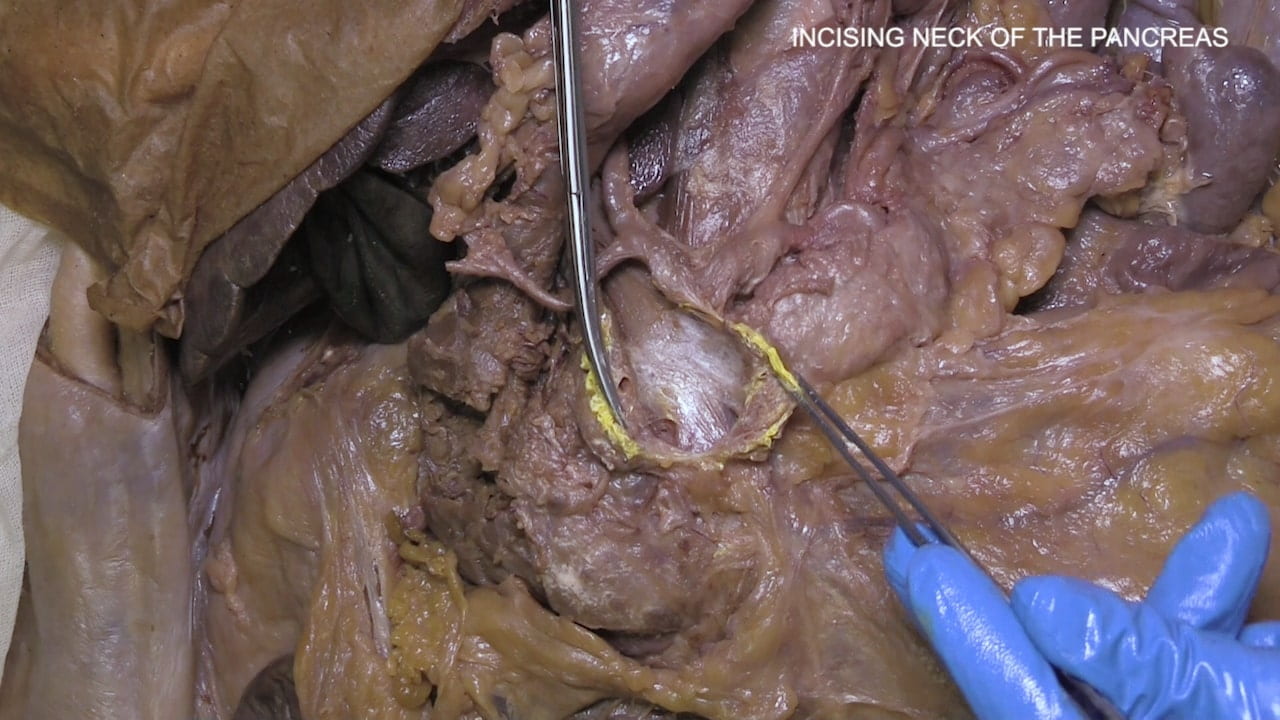
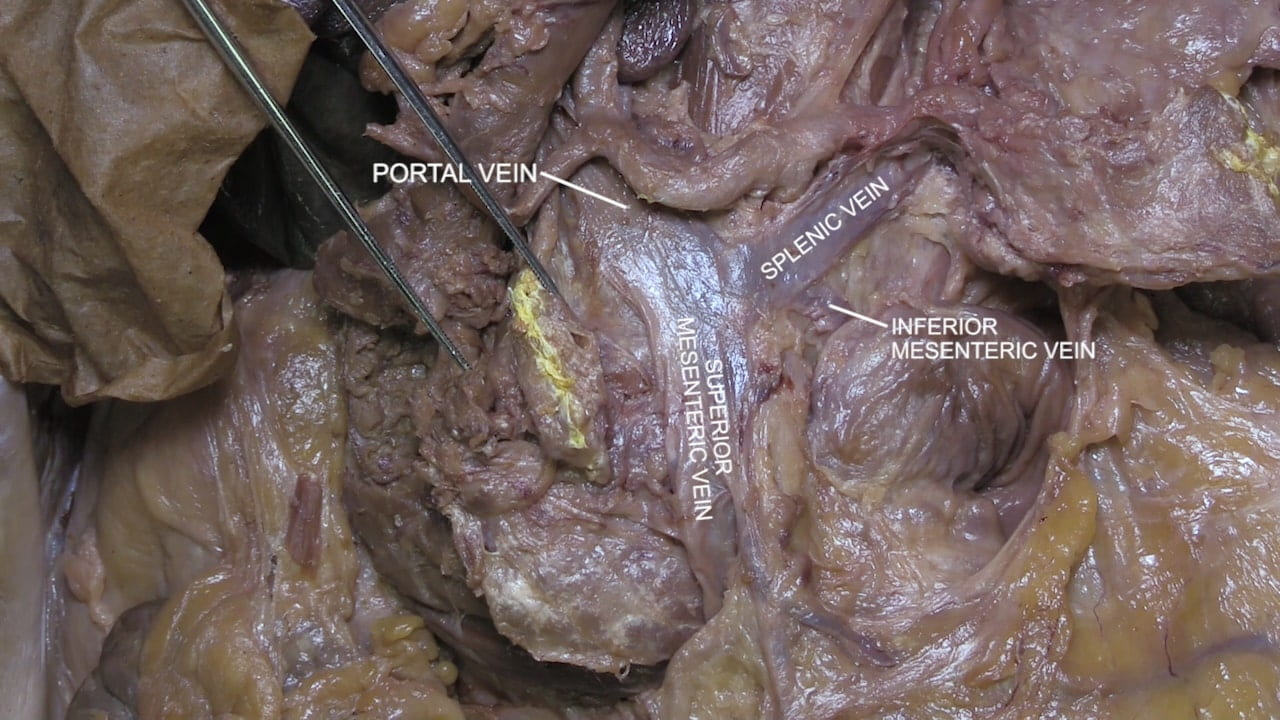
Follow the portal vein inferiorly by incising the neck of the pancreas.
Reflect the head and body of the pancreas laterally to view the formation of the portal vein from the union of the splenic and superior mesenteric veins.
Whipple Procedure
Upper Endoscopy, Harry Asianian
Duodenal Polyp Removal, Harry Asianian
Hepatopancreaticobiliary Tract Clinical Correlations
Trauma/EM: Liver Injury: The liver is commonly affected by penetrating and blunt force trauma to the abdomen. The liver is also prone to acceleration-deceleration injuries. Several anatomic features of the liver explain its susceptibility:
- Location/Size: highly anterior and large size increases risk of damage
- Fixation: several ligaments and the diaphragm hold regions of the liver in place, while others are more flexible; in the setting of acceleration, these various regions of the liver move at different rates
- Fragility: the liver’s parenchyma is very fragile, and Glisson’s capsule, which encapsulates the liver, is very weak
- Vascularity: the liver is highly vascularized so injuries to the parenchyma generally involve hemorrhage
There are many classification systems for liver injury but the most widely used is AAST Liver Injury Scale which grades according to extent of hematoma and parenchymal/vascular damage. Treatment ranges from non-operative management to open laparotomy; guidelines are complex and take grade of damage into consideration.
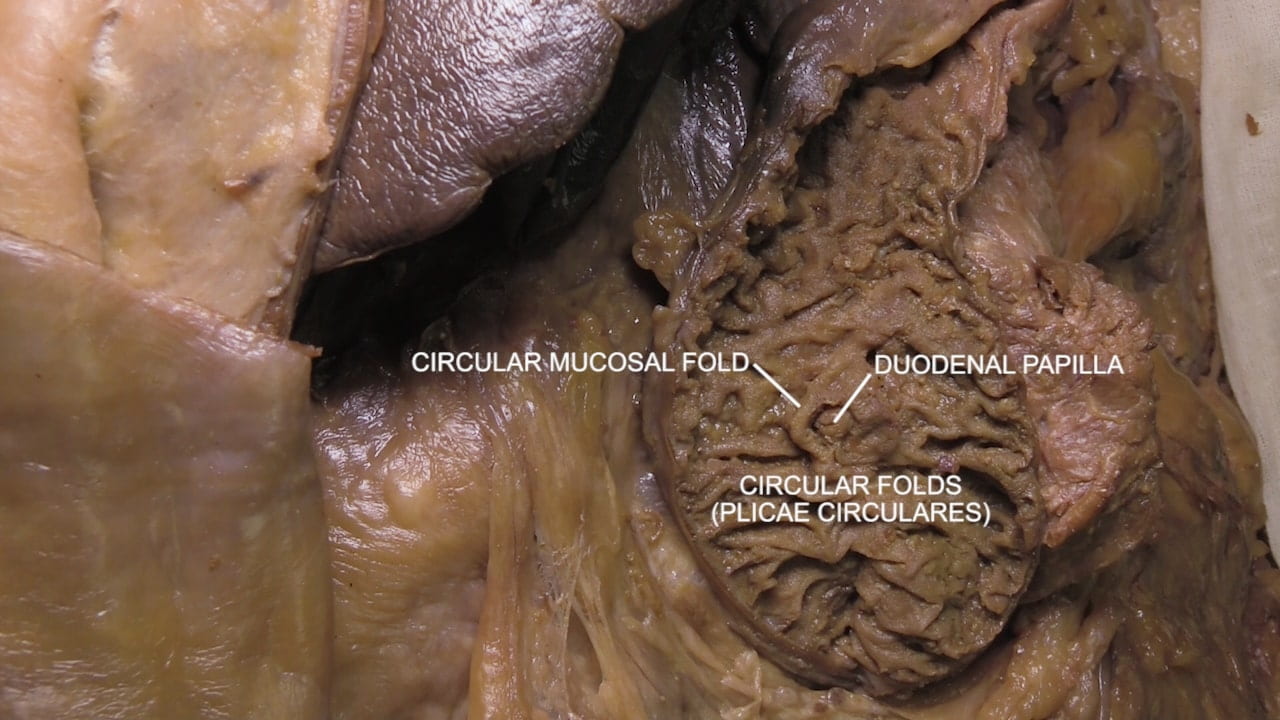
Procedure: ERCP: Recall that the main bile duct and the main pancreatic duct meet and drain through the major duodenal papilla into the second part of the duodenum; accessory pancreatic duct drains through the minor duodenal papilla. In cases where the major/minor duodenal papilla or the common bile duct/pancreatic ducts need to be accessed, an endoscopic camera (ERCP naming: Endoscopic) can be routed to the duodenum to access the duodenal papillae. Through the papillae, a variety of tools can be passed (ERCP naming: Retrograde). One important use of ERCP is visualization of the pancreaticobiliary tree (ERCP naming: Cholangiopancreatography) through cannulation of the papillae and injection of contrast dye (visualized by fluoroscopy). Importantly, a variety of additional maneuvers can be accomplished including stent placement, stone removal, biopsy, and intraductal ultrasound.
Embryology: Pancreas Divisium (PD): The embryological pancreas starts as two distinct buds from the duodenum; these outpouchings are the ventral and dorsal pancreas. The ventral bud is located near the gallbladder and has a duct (ventral duct) that connects to the common bile duct. The dorsal pancreatic bud contains a dorsal duct. At ~x days, the ventral bud rotates towards and eventually fuses with the dorsal bud. Ultimately, the dorsal bud becomes the tail, body, and a portion of the head of the pancreas; the ventral bud gives rise to the uncinate process and a portion of the head of the pancreas. Occasionally, the ventral and dorsal buds do not fuse yielding PD which is characterized by 1) a large dorsal pancreas that drains the majority of pancreatic secretions through the accessory pancreatic duct into the duodenum through the minor duodenal papillae, and 2) head and uncincate process (ventral pancreas) that drains bile and a small amount of pancreatic secretions into the major duodenal papillae. PD is the most common congenital abnormality, affecting ~10% of the population, and is usually asymptomatic. PD is generally detected incidentally during ERCP (see above) or other imaging modalities.
Surgery/Autopsy: Whipple Surgery: In cases of malignancy (or trauma/pancreatitis) necessitating removal of the pancreas head/uncinate process or the distal biliary tree, a pancreaticoduodeenectomy (AKA Whipple Surgery) is performed. Importantly, this operation is quite complex necessitating several maneuvers (also see image below):
- Depending upon tumor infiltration severity, a portion of the distal stomach may be removed
- To ensure complete removal of tumor, the gallbladder and much of the distal bile duct is removed
- The head of the pancreas is removed, which necessitates removal of the duodenum due to shared blood supply
- The biliary tree, pancreas, and stomach are all independently anastomosed with the remaining jejunum
Common complications following this surgery include delayed gastric emptying (secondary to nerve damage or mechanical considerations), bile leak, and pancreatic leak. An important consideration in determining whether a patient’s tumor is amenable to a Whipple is involvement of vasculature (THINK: what vasculature is near the pancreas? Ask in lab).
Anatomical Variations: Cystic Duct and Artery Variations: The cystic artery arises from the right hepatic artery in most of the population; from this cystic artery, superficial and deep branches arise. However, several variations are also common:
- superficial and deep branches of the cystic artery may not arise from the same origin (i.e., double cystic artery)
- cystic artery can branch from the left hepatic artery (may travel to gallbladder through liver parenchyma or cholecystocolic ligaments)
- cystic artery can branch from the gastroduodenal artery (i.e., low-lying cystic artery)
- cystic artery can come off the left hepatic artery.
~4% of the population will undergo cholecystectomy, during which the cystic artery must be identified and ligated, so knowledge of the different variations is critical.
Imaging: In addition to the general abdominal imaging techniques introduced last week, targeted imaging can be performed of the liver and biliary system. Ultrasound is excellent for evaluating the gallbladder and looking for biliary ductal dilatation. CT is usually the next step in evaluating the liver or pancreatic parenchyma (including the associated vasculature) for abnormalities such as tumors, injury or infection/inflammation. When needed, MRI can help further characterize soft tissue lesions in the liver and pancreas, and is also very effective at evaluating biliary ductal anatomy and abnormalities such as dilation/obstruction or inflammation. Interventional gastroenterologists utilize endoscopy for direct visualization and treatment of the biliary tree (see ERCP above), and use endoscopic ultrasound for evaluation and targeted biopsy of pancreatic lesions.
Imaging Correlate: See imaging of an inflamed liver cyst at Table 7.
Images (Click to Enlarge)


Autopsy photos showing liver injuries sustained from descent from height (left) and motor vehicle collision (right)


Left: pancreas and duodenum specimen taken from patient who underwent Whipple (* = pancreatic head); Middle: serially sectioned pancreatic head showing tumor (arrow); Right: High power image of tumor, adenocarcinoma composed of malignant glands in fibrotic stroma