Assigned Female Pelvis
Lab Summary
The structure of the female pelvis and the perineum along with their contents are taught. The female pelvis and perineum are presented from external structures to pelvic contents. Additionally, the female pelvis is shown from a midline sagittal perspective. The course of retroperitoneal vessels and nerves are demonstrated.
Lab Objectives
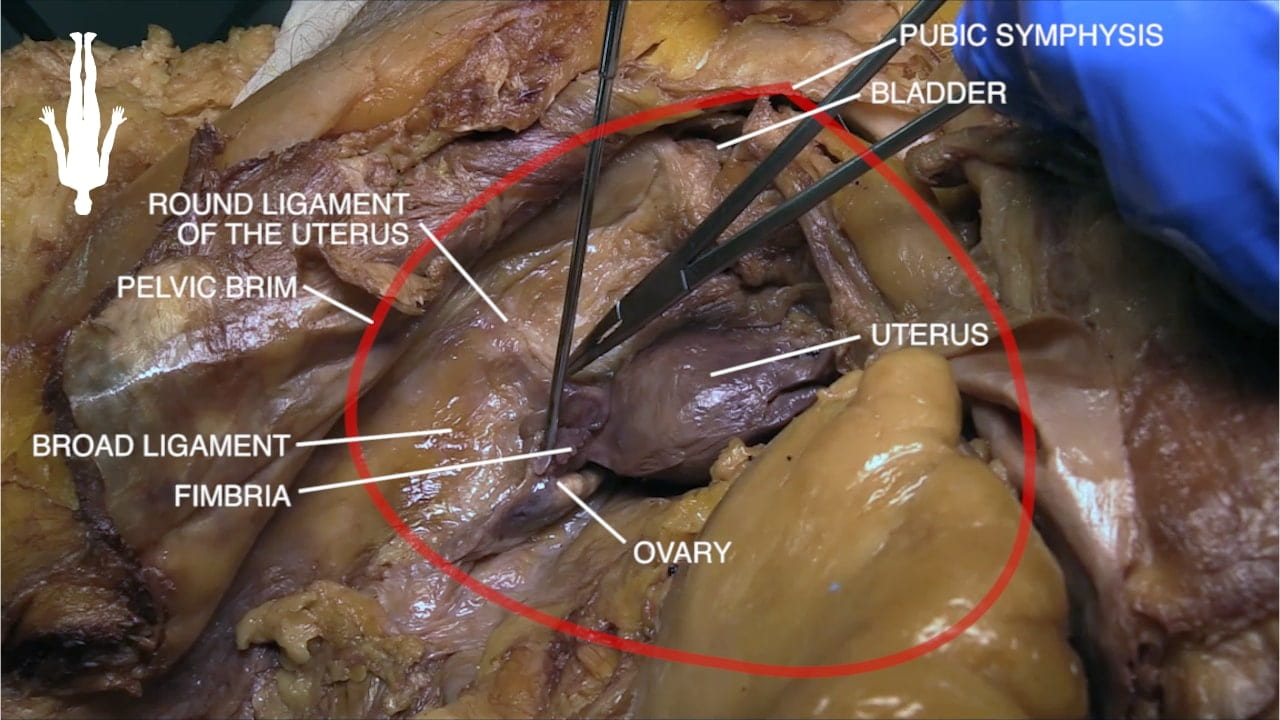
- Name structures in broad ligament.
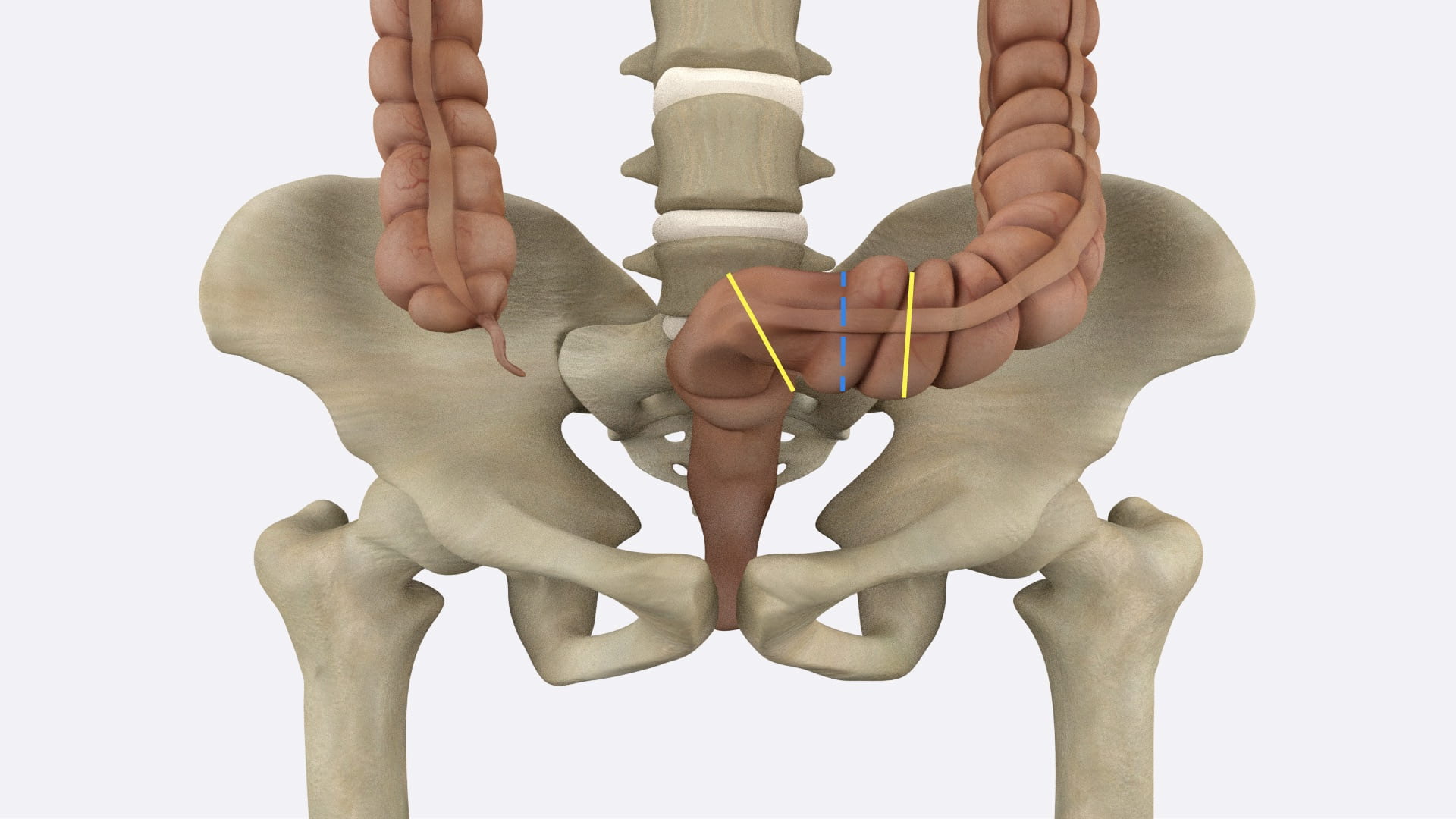
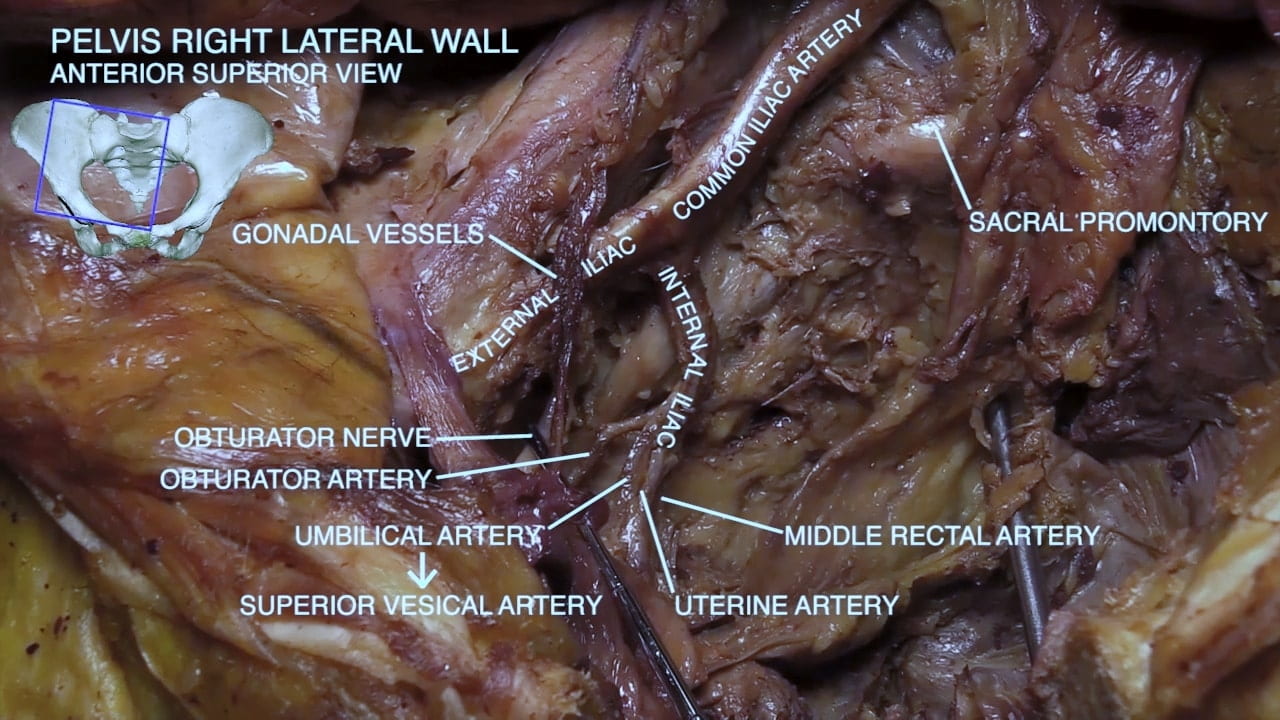
- Describe relationship between uterine artery and ureter.
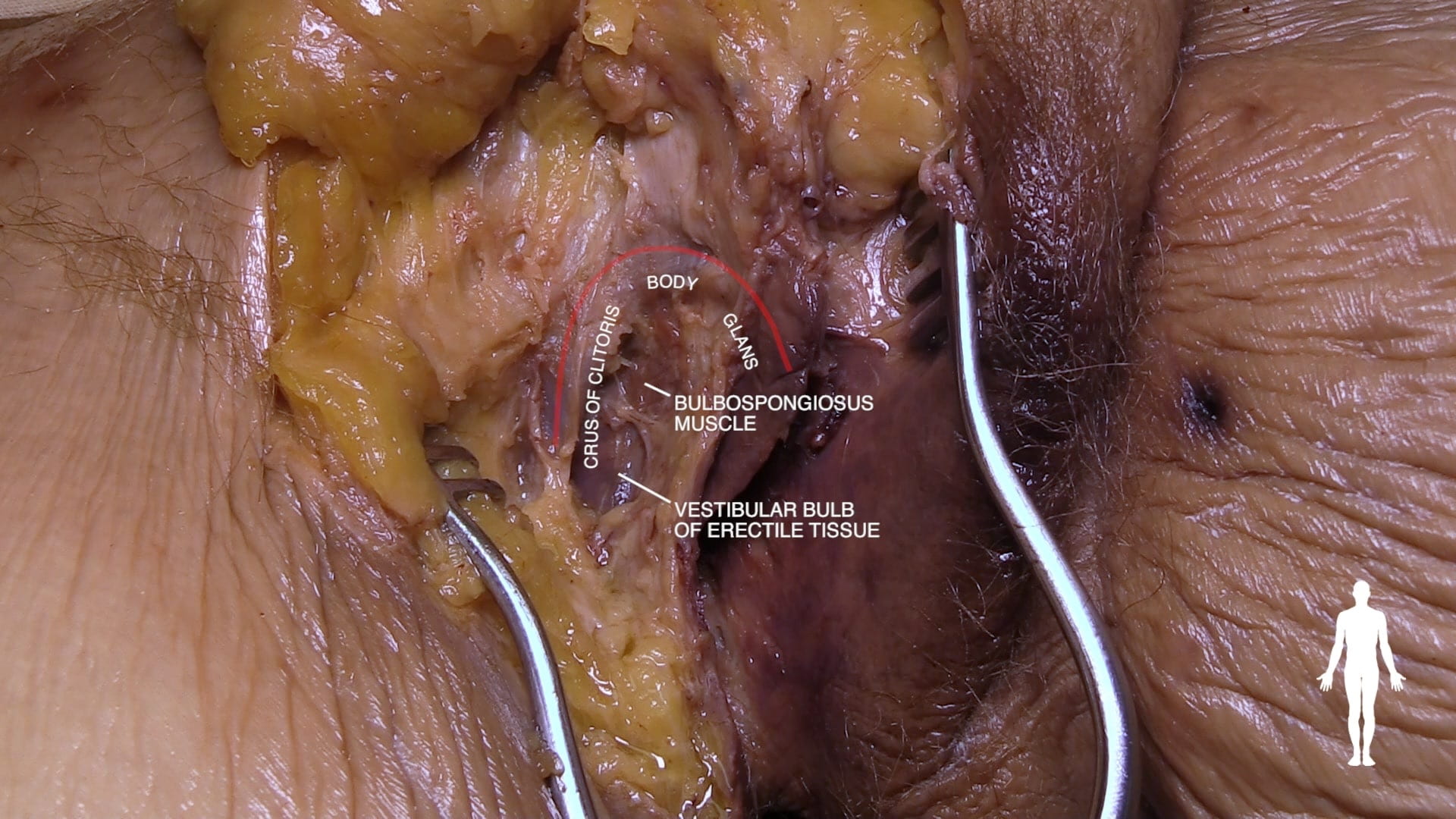
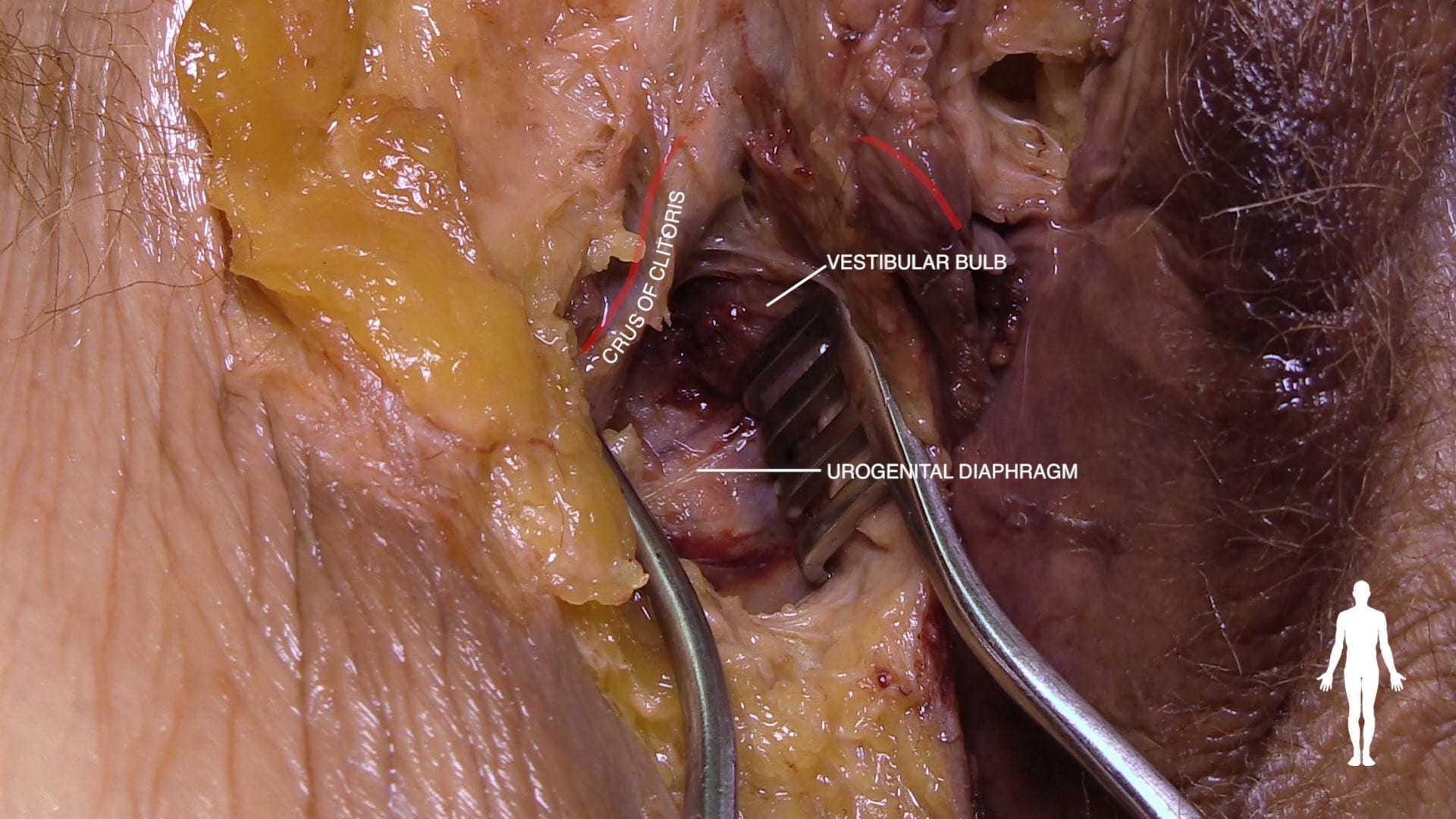
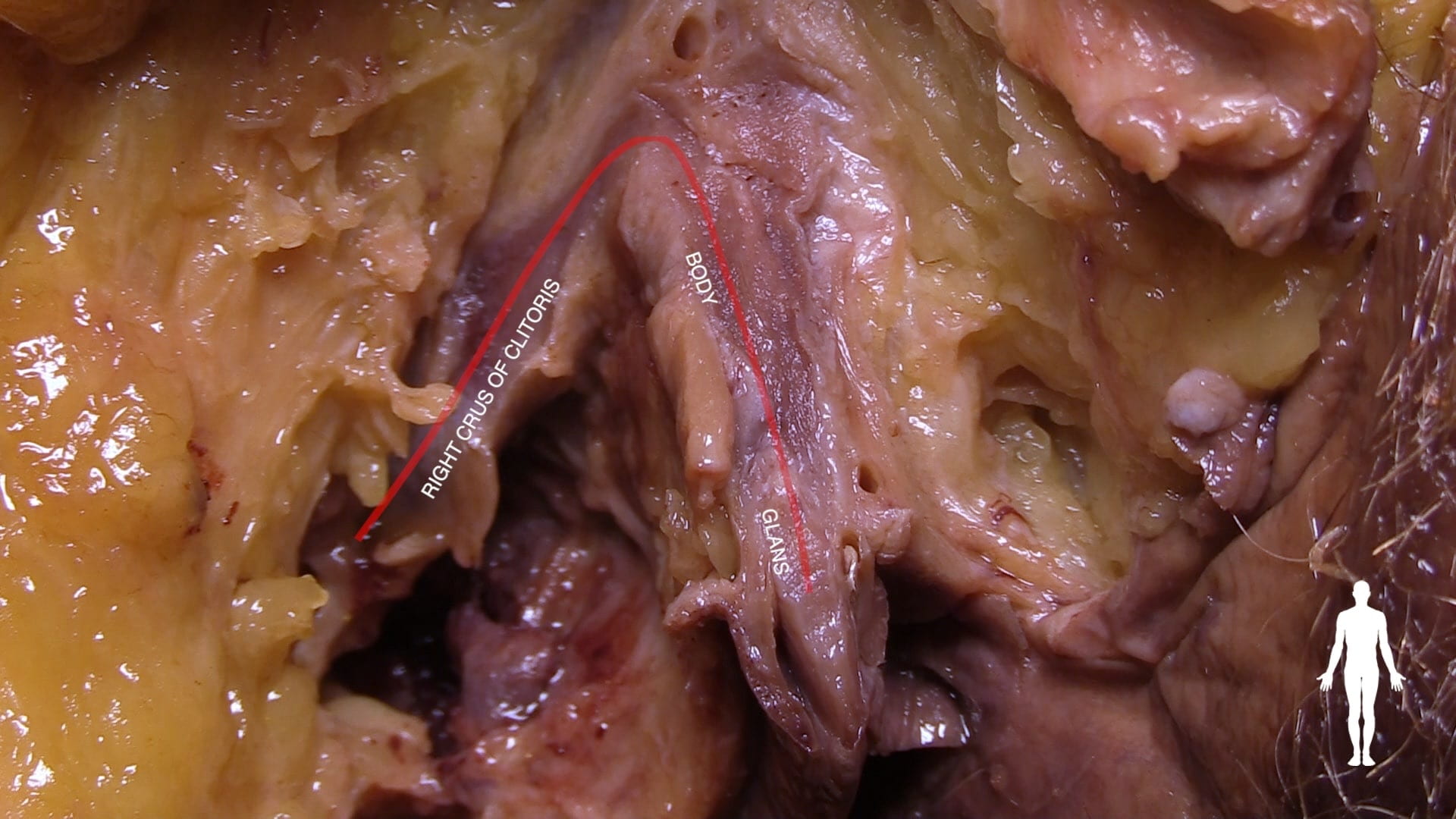
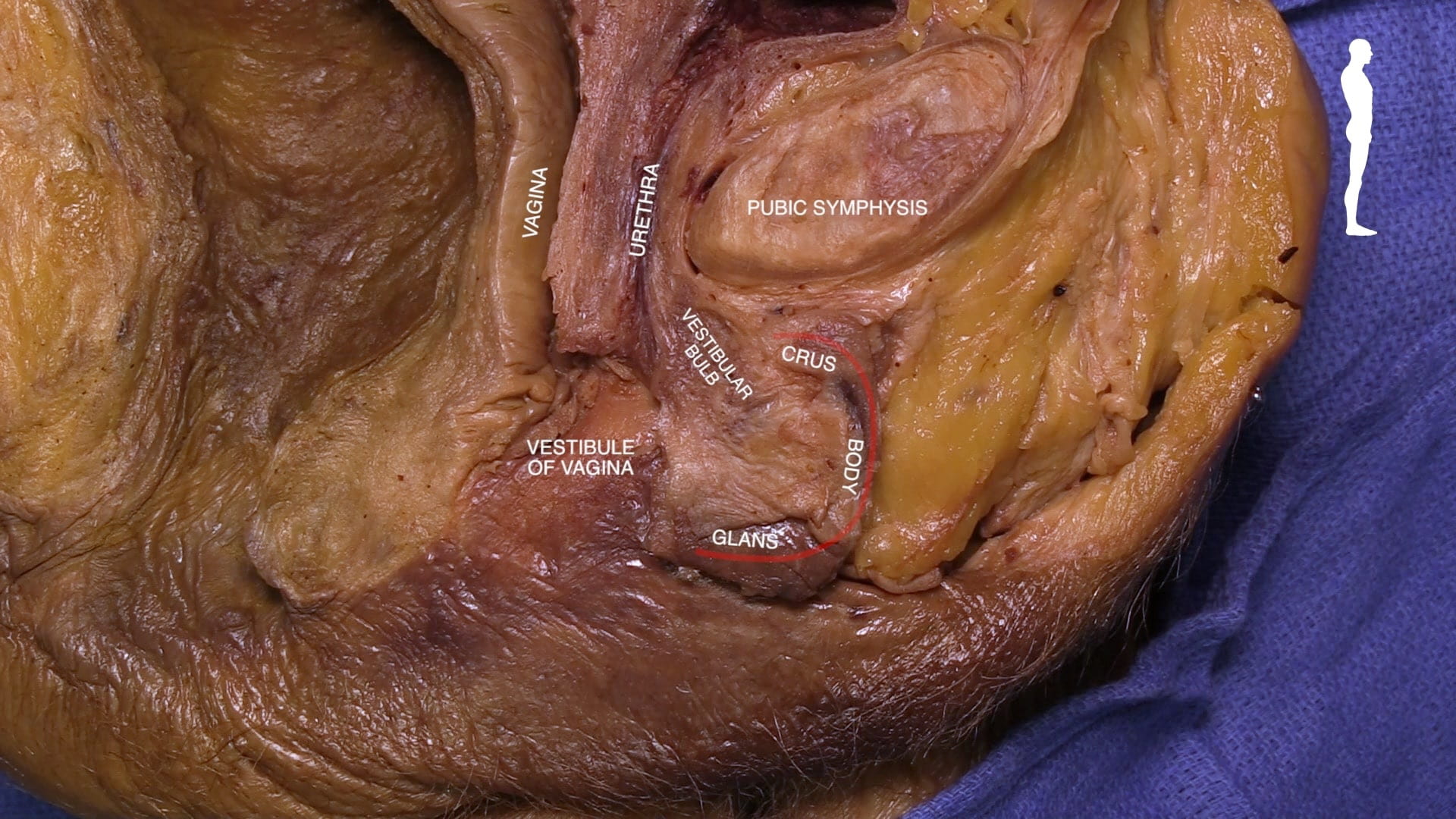
- Describe positions of glans and crus of clitoris and vestibular bulb.
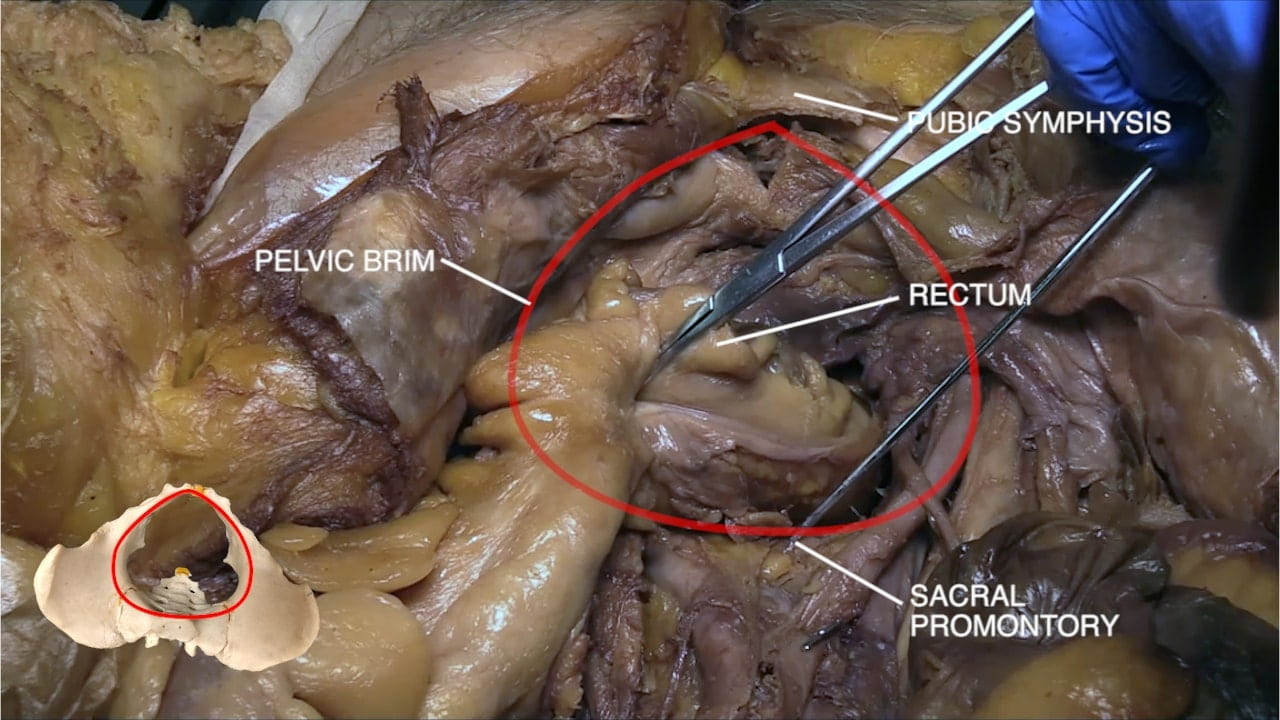
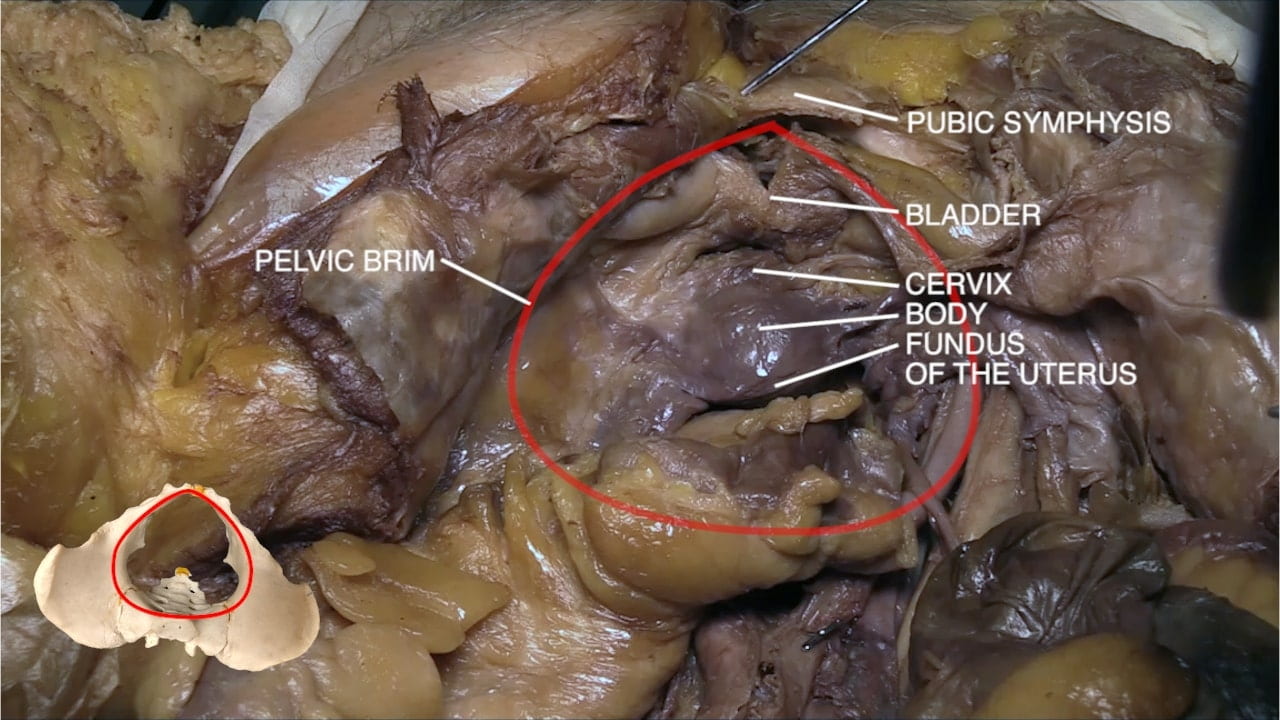
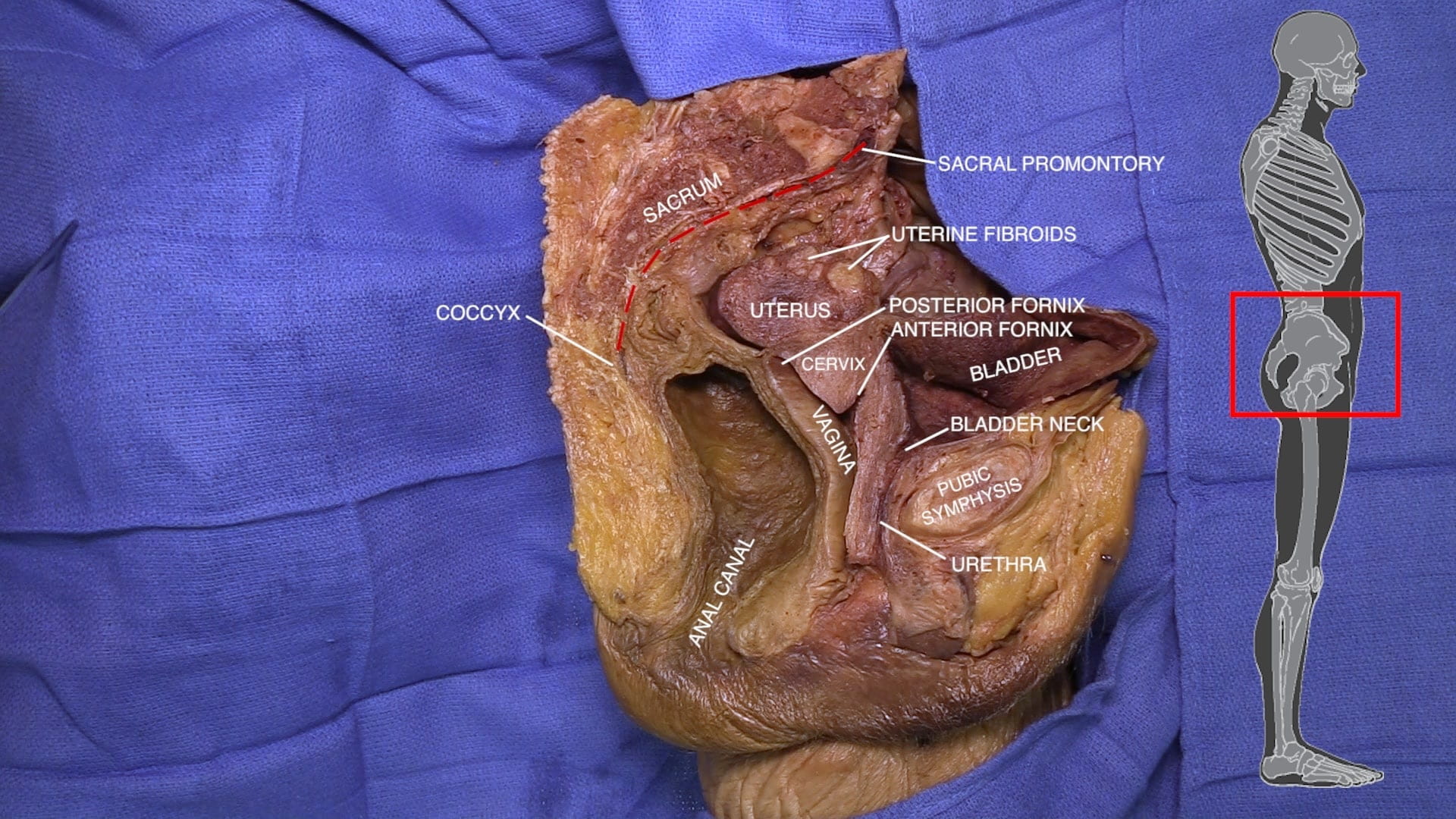
- Name principal structures in midline pelvis of female.
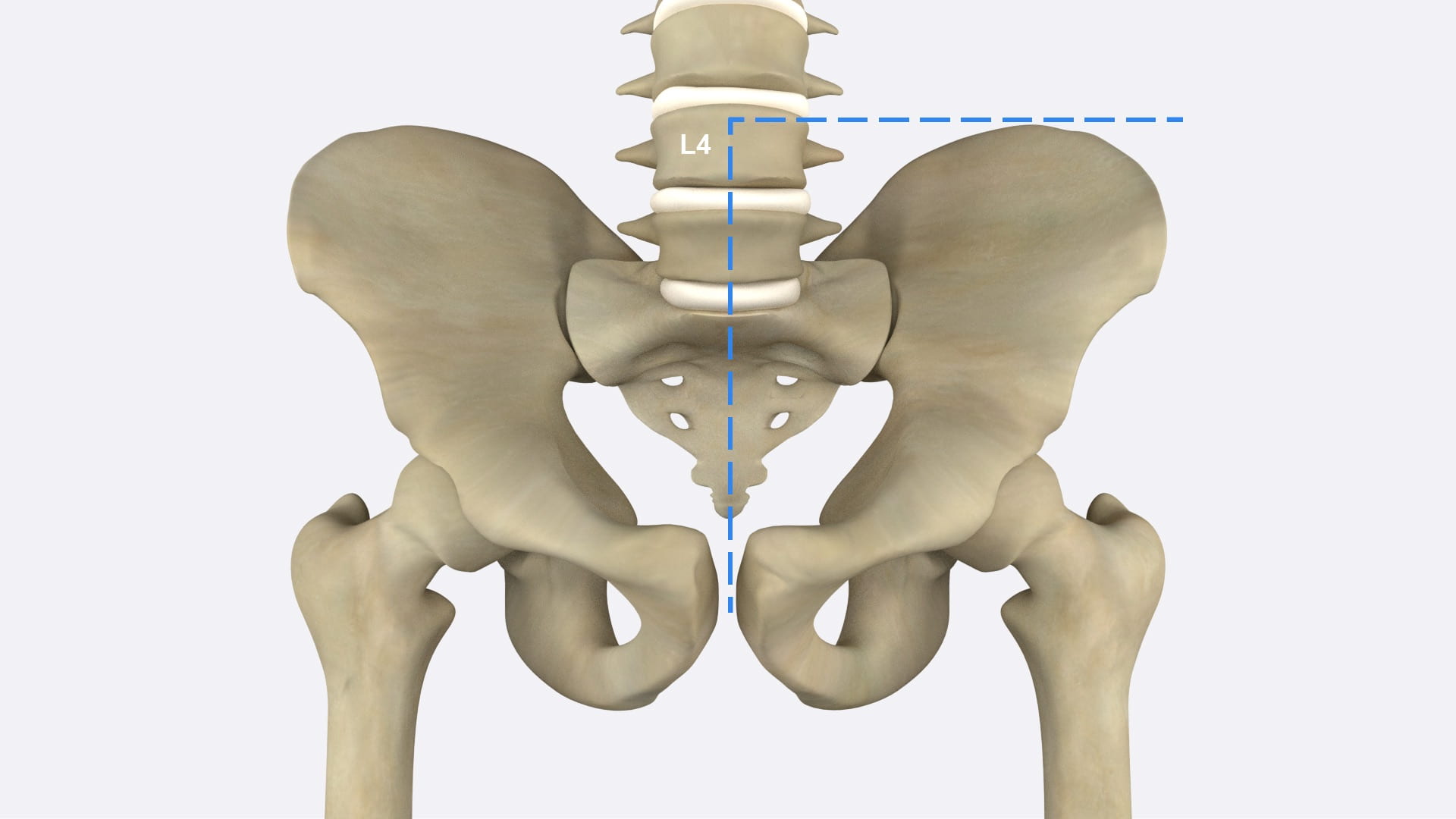
- Describe A-P dimension of pelvic inlet and how it is estimated.
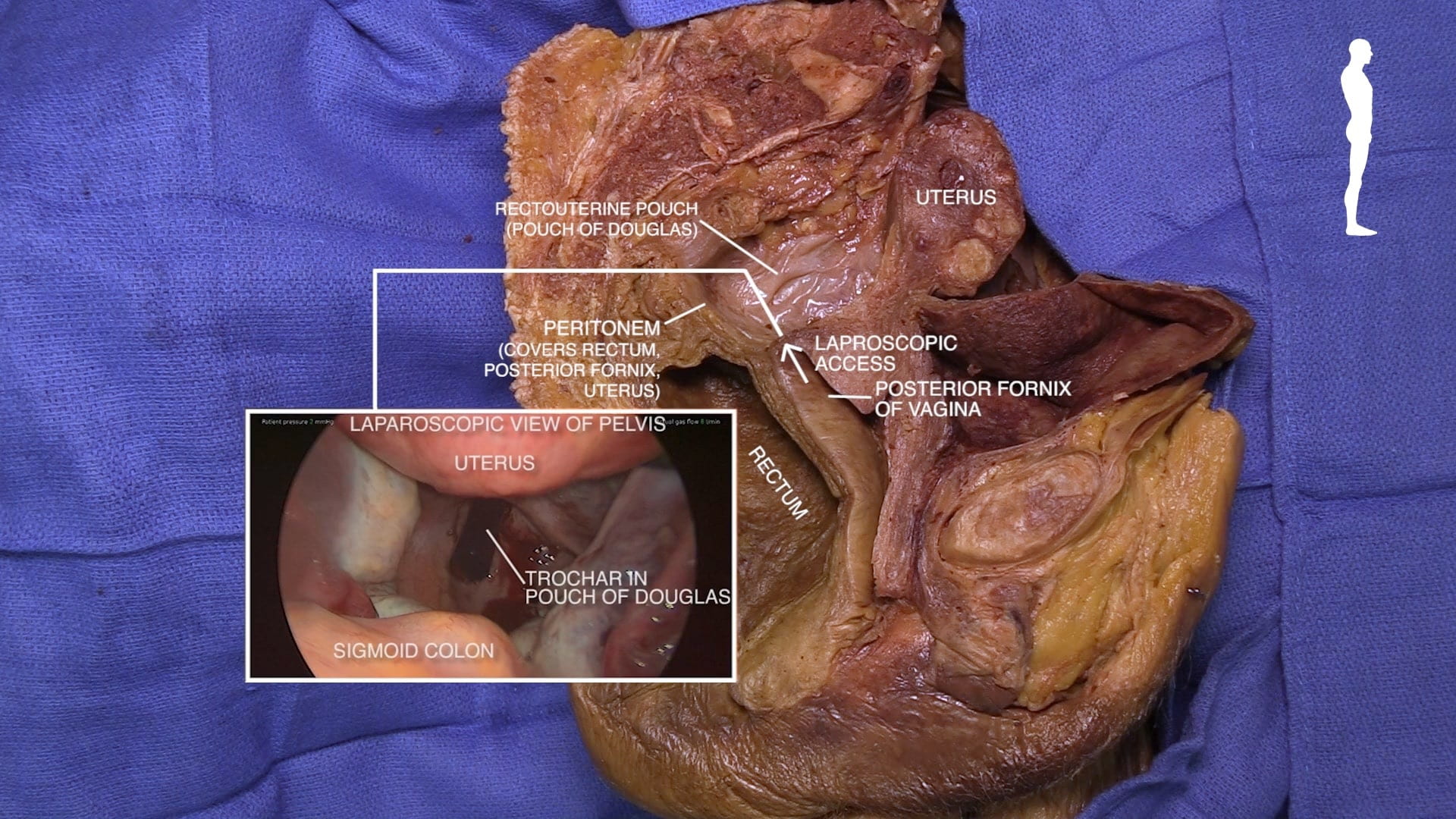
- Explain clinical importance of posterior fornix of vagina.
- Describe diagonal conjugate.
- Describe the erectile tissue of clitoris and vestibular bulb.
Lecture List
Female Perineum, Female Pelvis, Female Sagittal Pelvis, Pelvic Vessels and Nerves
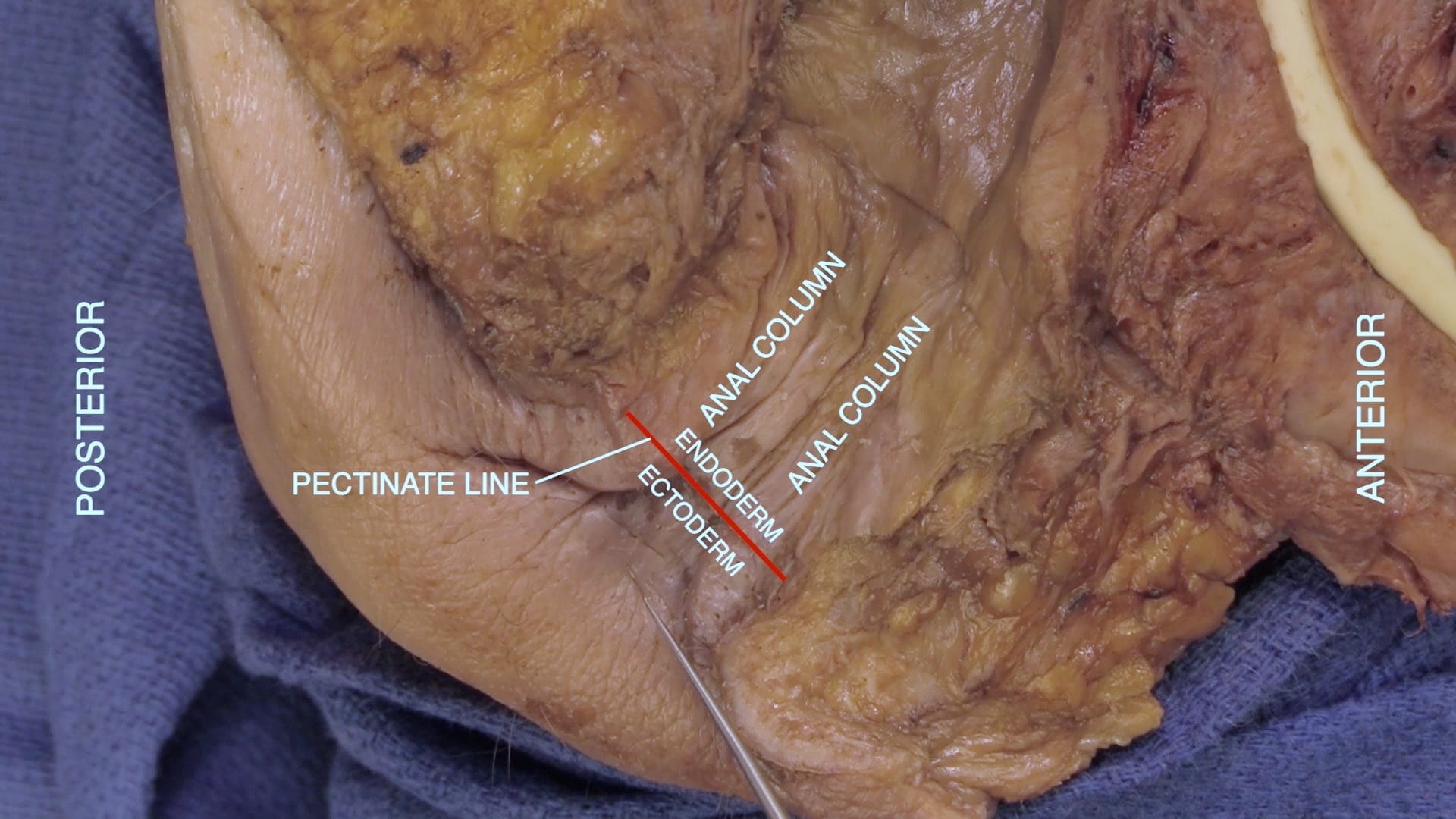
Female Perineum
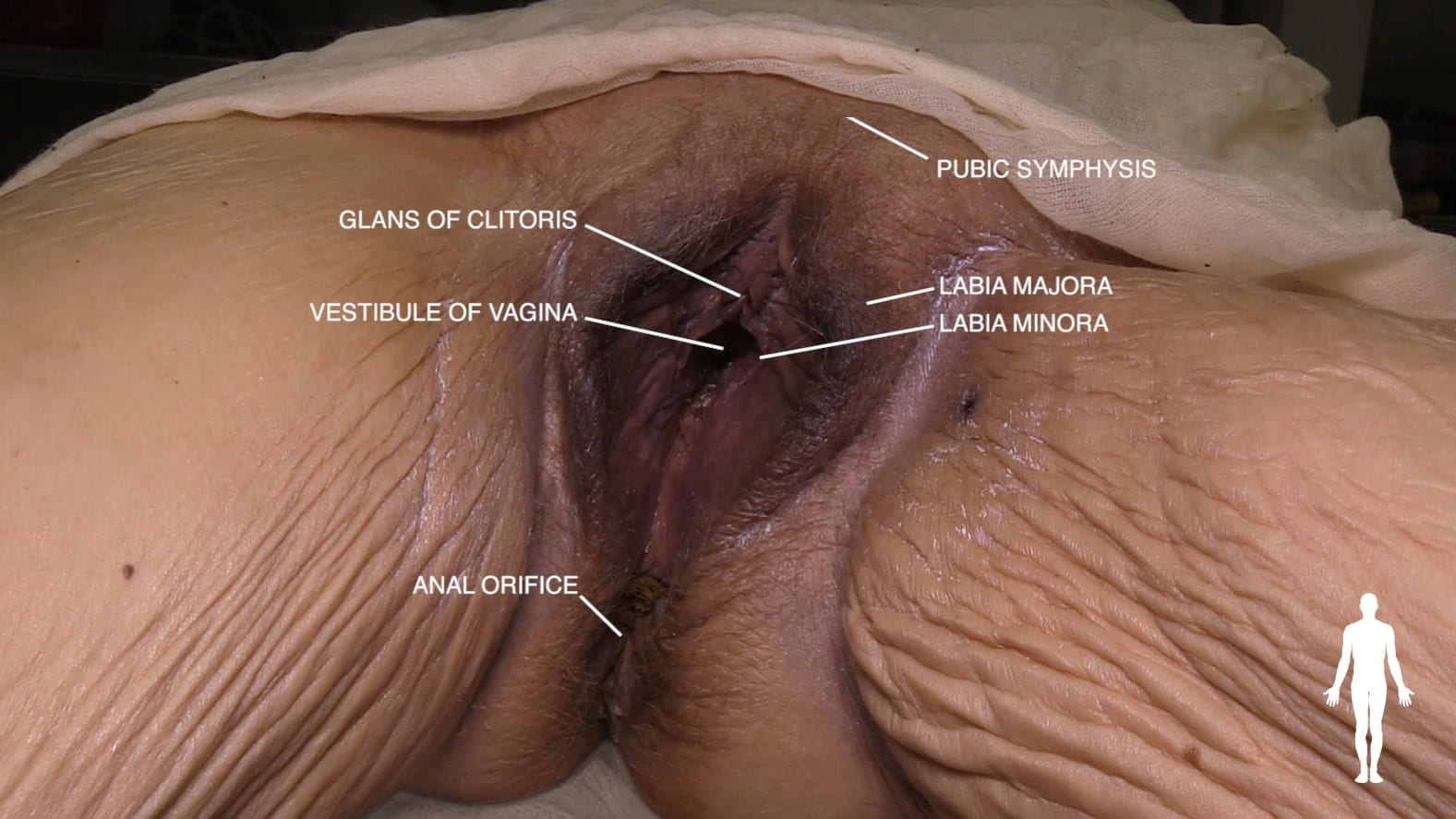
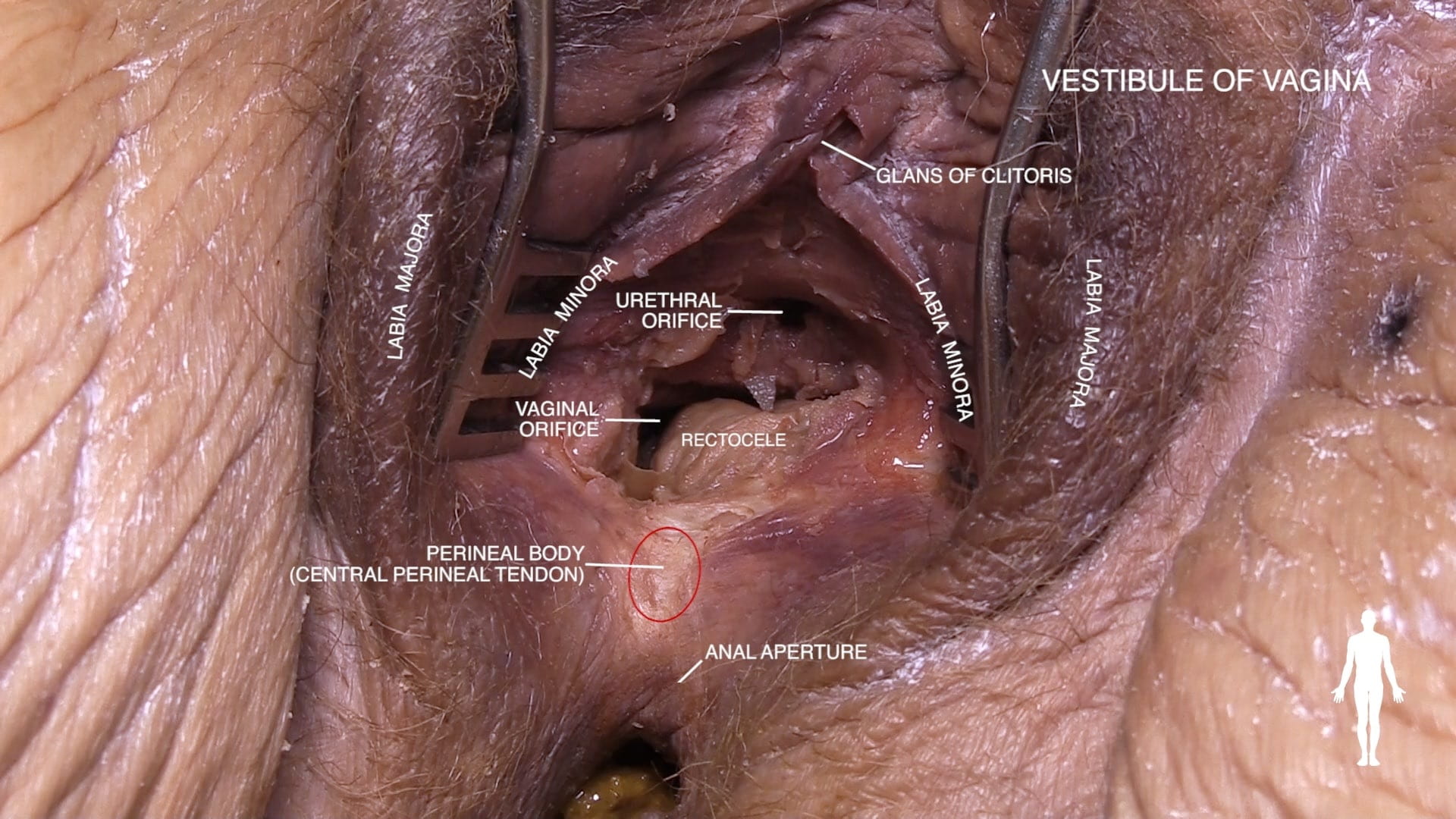
External Genitalia
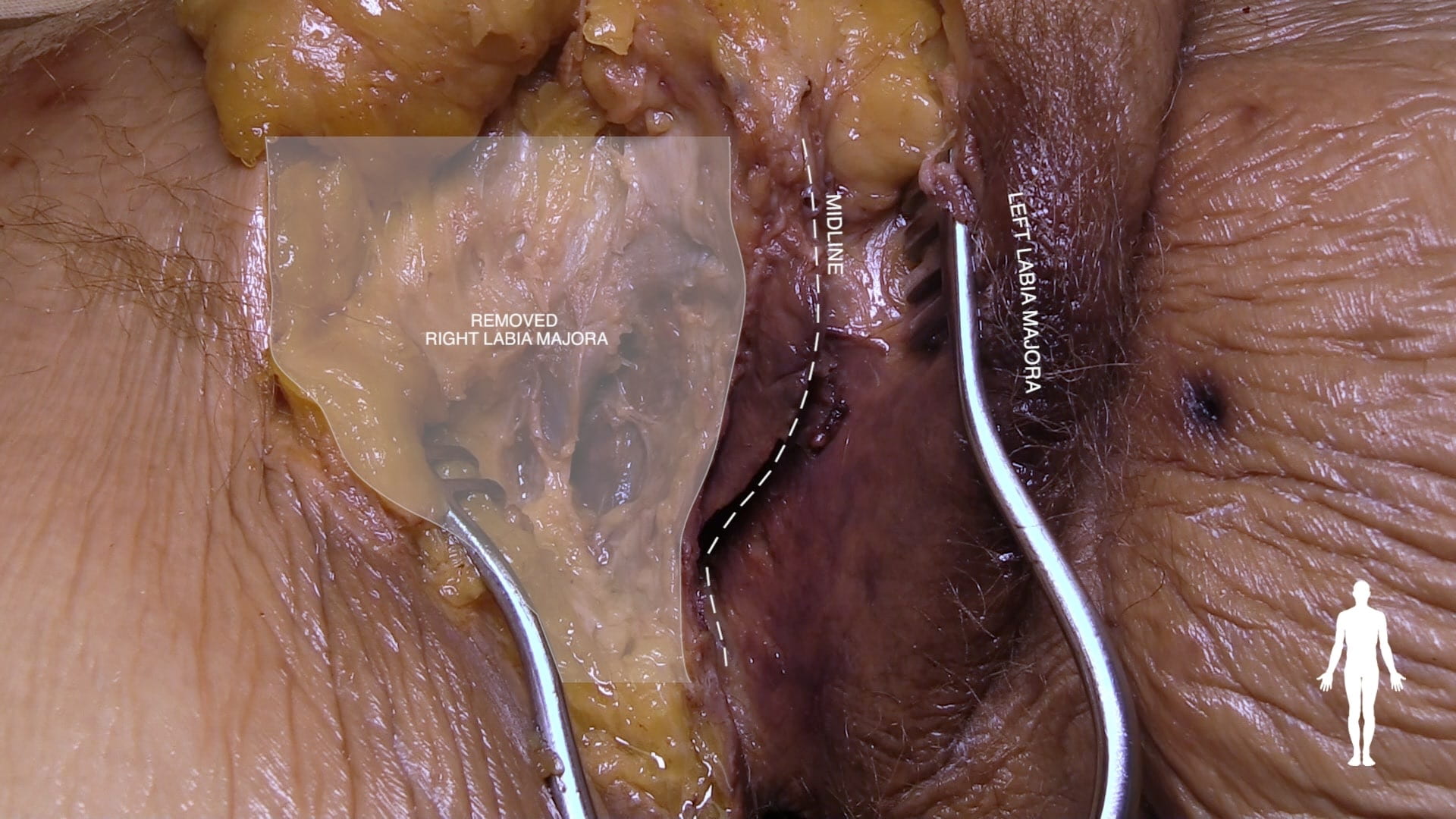
Erectile Tissue
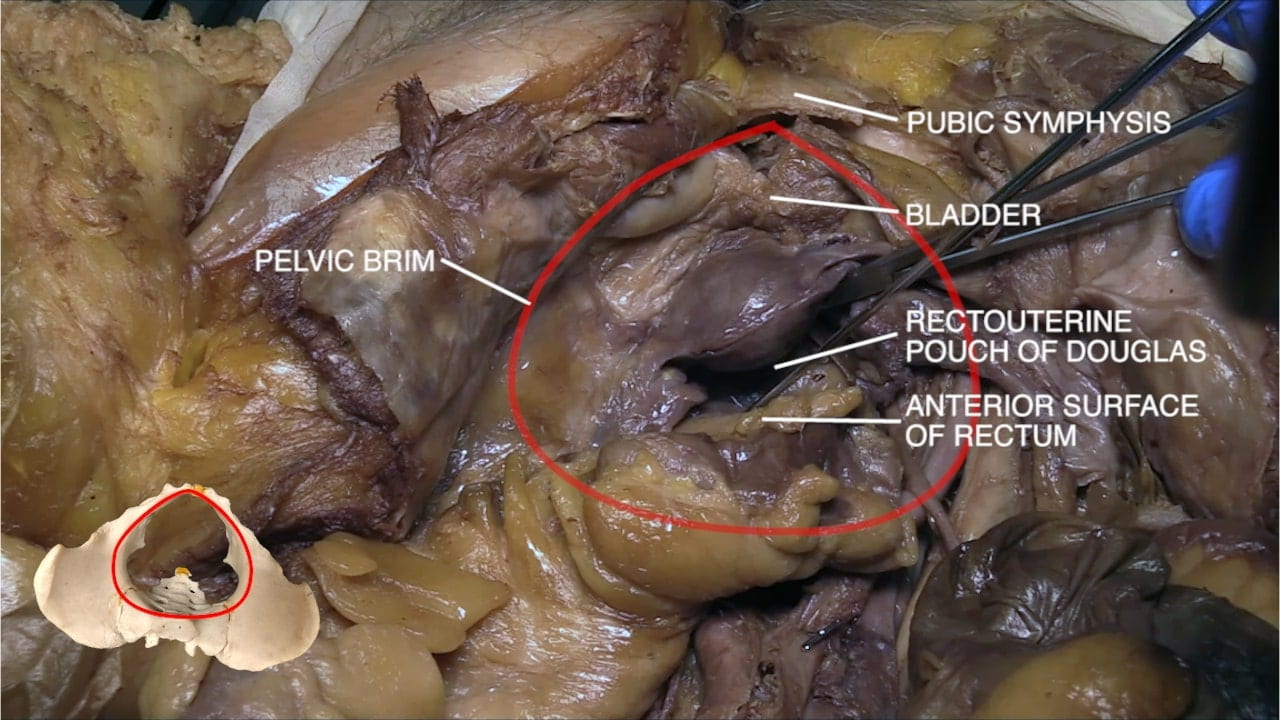
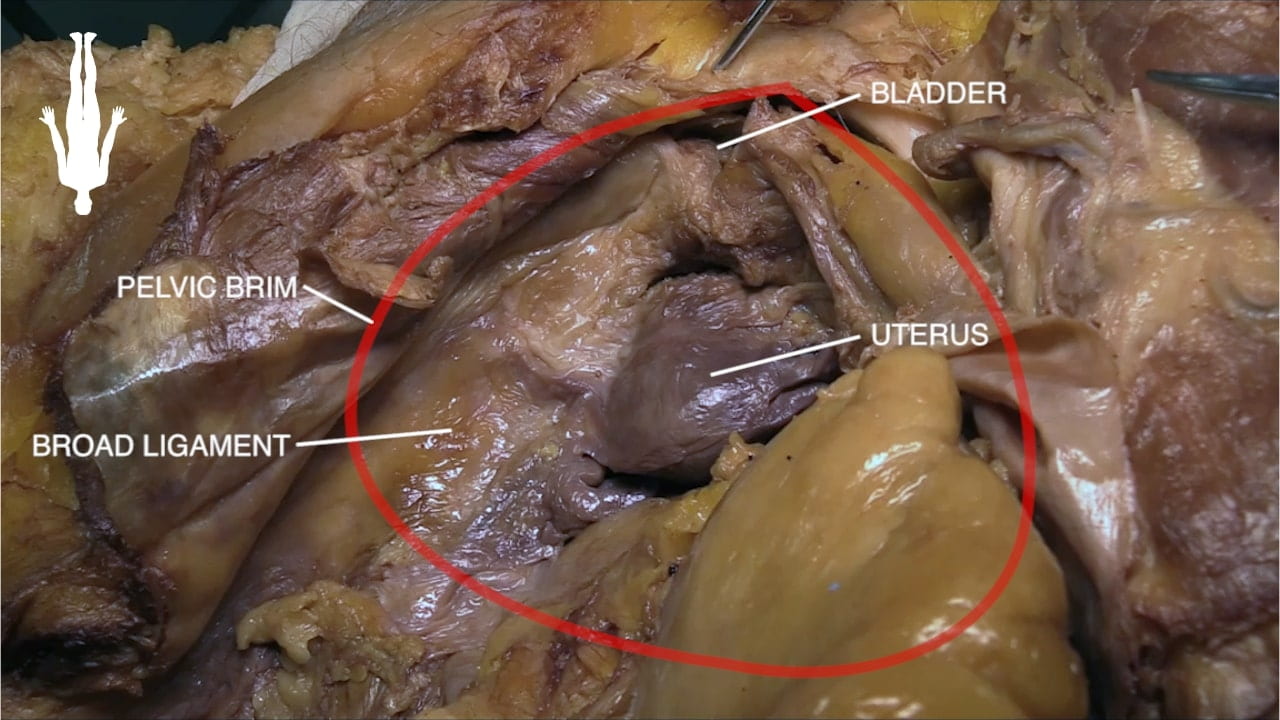
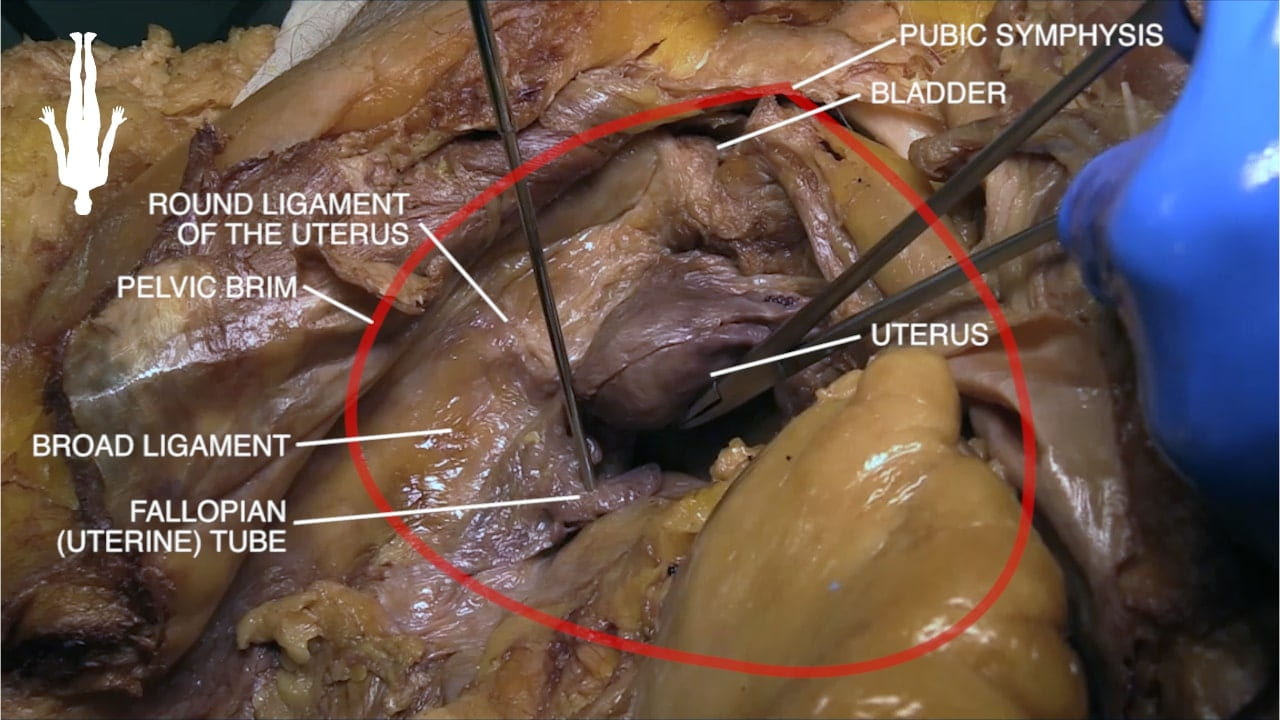
Female Pelvis
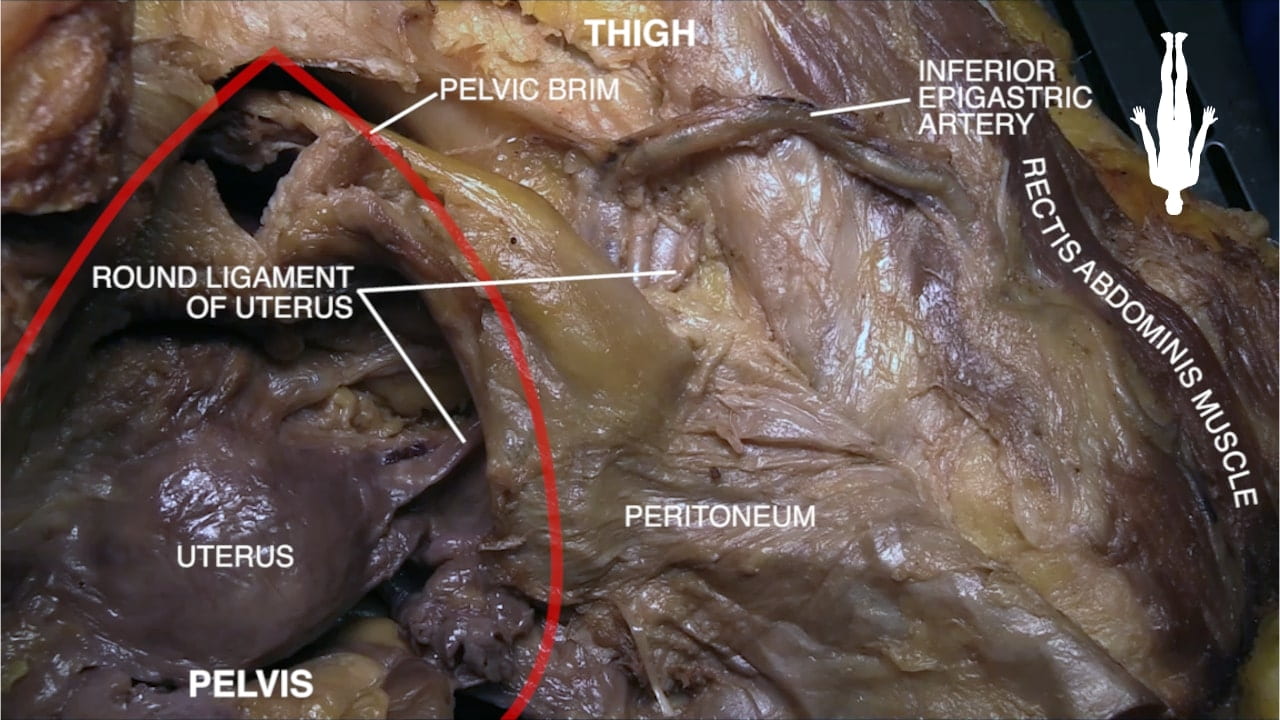
Uterus
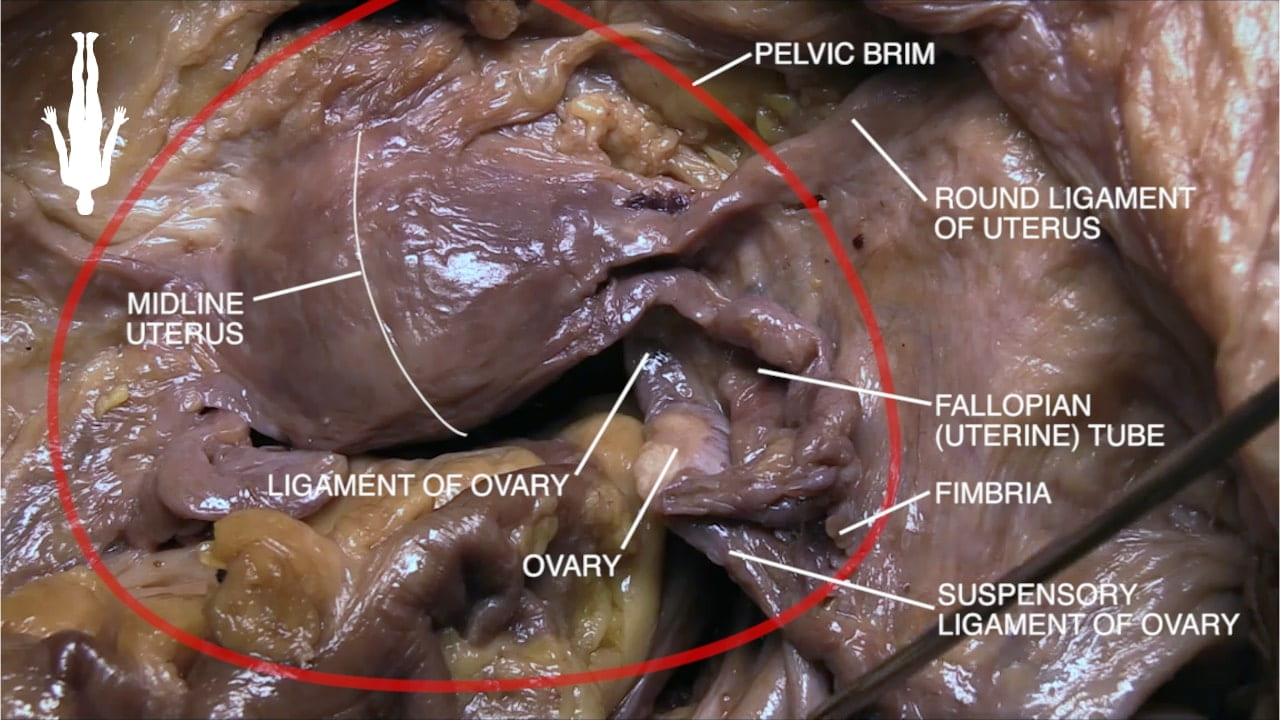
Uterine Adnexa
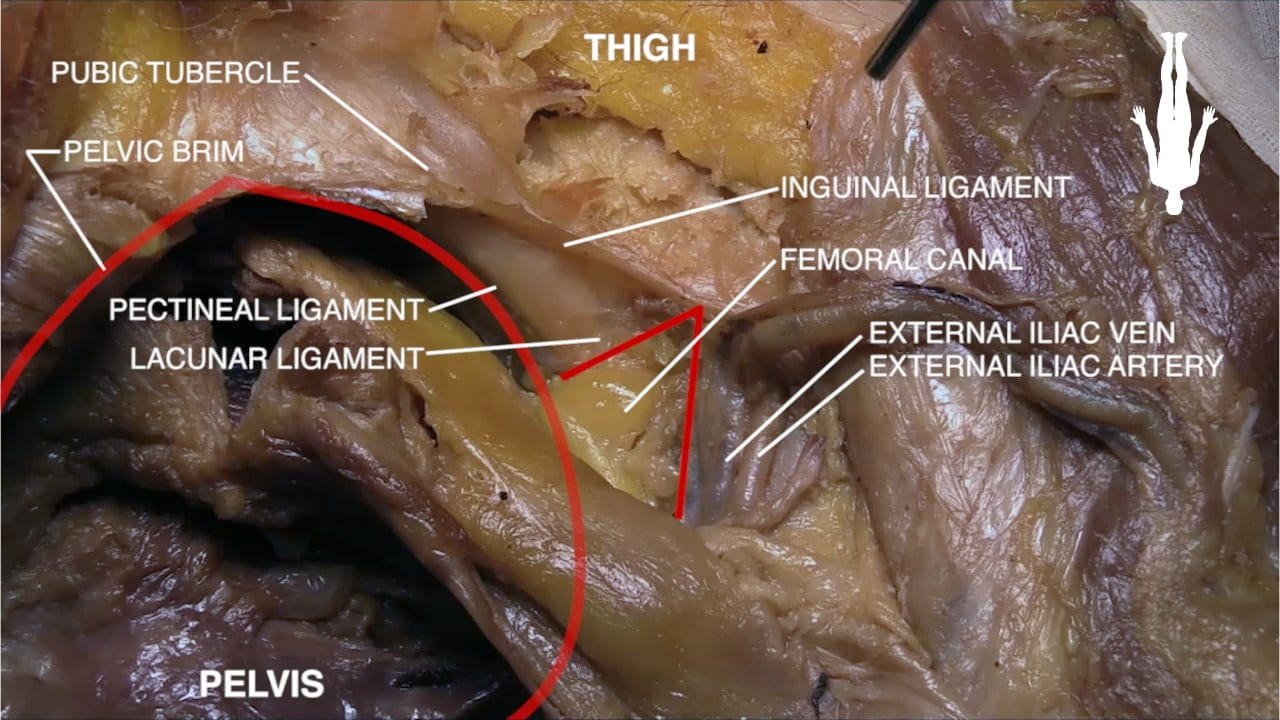
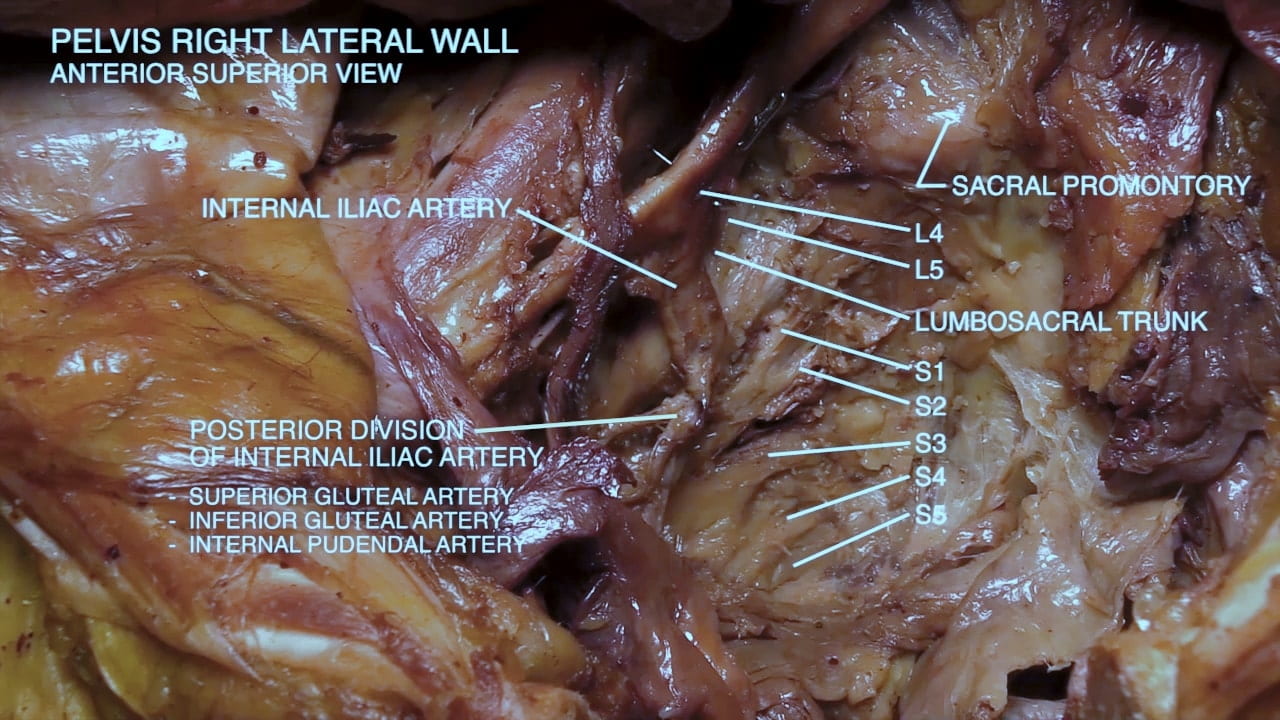
Iliac Vessels and Femoral Canal
Key Sagittal Pelvic Dissection Notes
- Split pelvis
- If no split, perineum in AFAB is difficult – try separating legs progressively with blocks to hold them apart.
- For AFAB with uterus, try a hysterectomy with Ob-Gyn – laparoscope may be helpful for visualizing deep structures. Note relationship of uterine artery and ureter.
- For all, examine pelvic vasculature, course of ureter and lumbosacral plexus.